Medical record

BCMS Pat Sharma
President’s Scholarship Recipients:
Outcomes in Solid Organ Transplant Patients Receiving Immune Checkpoint Inhibitors by Cyrus Rahmanian
Dysbiosis and Anxiety: Evidence for Association, Gut-Brain Axis Mechanisms and Intervention Strategies by Emily Shirk
INSIDE:
Respiratory Specialists is the region’s largest and most respected pulmonology group, staffed by board-certified pulmonologists and advanced practice providers with subspecialty expertise in pulmonary and sleep medicine. We offer comprehensive diagnostic evaluations, evidencebased treatment protocols, and longitudinal management for a wide range of respiratory and sleep disorders. Our collaborative approach ensures continuity of care and timely communication with referring providers.
• Sleep Evaluation (OSA, narcolepsy, insomnia,restless legs syndrome)
• Spirometry
• Biologics Treatment for Asthma
• Interstitial Lung Disease
• Occupational Lung Disease

• Pulmonary Hypertension
• Lung Nodule Surveillance
• Lung Cancer
• Robotic-Assisted Bronchoscopy
• Endobronchial Ultrasound
• Clinical Research Trials


Medical record
A Quarterly Publication
To provide news and opinion to support professional growth and personal connections within the Berks County Medical Society community.
Berks County Medical Society MEDICAL RECORD
D. Michael Baxter, MD, Editor
Editorial Board
D. Michael Baxter, MD
Lucy J. Cairns, MD
Daniel Forman, DO
Shannon Foster, MD
William Santoro, MD
Raymond Truex, MD
Beth E. Gerber, IOM
Berks County Medical Society Officers
Ankit Shah, MD President
Olapeju Simoyan, MD President Elect
Daniel Edwards, DO Treasurer
William Santoro, MD
Immediate Past President Secretary & Delegation Chair
Directors
Advocacy Chair: D. Michael Baxter, MD
Collegiality Chair: Pauletter Dreher, DO
Early Career Physician Chair: Caitlyn Moss, MD
Education Chair: Lucy Cairns, MD
Medical Record Editor: D. Michael Baxter, MD
Medical Student Chair: Peter Aziz (one-year term)
Residency Chair: Fatima Khalid, MD (one-year term)
Eve Kimball, MD
Jacob Lucas, DO
Amogh Nagol, student (one-year term)
Osadebamwen ‘Deb’ Osaghae, MD, resident (one-year term) Wei Shaw, DO
Mansi S. Vasconcellos, MD*, BCMS Alliance President Staff
Beth E. Gerber, IOM Executive Director
* designates non-voting member
Berks County Medical Society
2669 Shillington Rd., Suite 501, Sinking Spring, PA 19608 (610) 375-6555 • (610) 375-6535 (FAX) info@berkscms.org • www.berkscms.org
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Berks County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Berks County Medical Society.
Manuscripts offered for publication and other correspondence should be sent to 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. The editorial board reserves the right to reject and/or alter submitted material before publication. The Berks County Medical Record (ISSN #0736-7333) is published four times a year by the Berks County Medical Society, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. Subscription $50.00 per year. Periodicals postage paid at Reading, PA, and at additional mailing offices.
POSTMASTER: Please send address changes to the Berks County Medical Record, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501.


Berks County Medical Society –BECOME A MEMBER TODAY! Go to our website at www.berkscms.org and click on “Join Now” 27 Berks County Medical Society Historical Center Dedicated in the Reading Hospital
Advances in Urology: Newer Diagnostic & Treatment Options for Prostate Disease
Berks County Medical Society Alliance Celebrating 100 Years of Service
2025 BCMS Night at the Reading Fightin’ Phils
School Absenteeism and How Physicians Can Help
Student Vital Signs
Content Submission: Medical Record magazine welcomes recommendations for editorial content focusing on medical practice and management issues, and health and wellness topics that impact our community. However, we only accept articles from members of the Berks County Medical Society. Submissions can be photo(s), opinion piece or article. Typed manuscripts should be submitted as Word documents (8.5 x 11) and photos should be high resolution (300dpi at 100% size used in publication). Email your submission to info@berkscms.org for review by the Editorial Board. Thank YOU!

Ankit Shah, MD, FACEP, FAAEM, FAMIA President

Family. Friends. Community.
All three were on full display at the BCMS picnic at the R-Phils game. I had a great time chatting with physicians from across specialties—hospitalists, ophthalmologists, and many more. Just as energizing was connecting with the next generation—our residents and students. The enthusiasm was contagious (the free food didn’t hurt either!). The game was exciting, the weather couldn’t have been better, and I even got to throw out the first pitch (a little inside, but absolutely a strike!).
As you flip through this issue, pay special attention to the student articles. Every year I’m in awe of the incredible work “these kids” are producing—far beyond what I could have pulled off at their age (and maybe even today). Their creativity and perspective are inspiring, and their minds seem to operate on levels I couldn’t begin to grasp back when I was in training.
A quick reminder: BCMS and PA Med membership renewal is underway. Please renew at your earliest convenience and encourage colleagues in your practice who aren’t yet members to join. As a thank-you for your dedication to medicine here in Berks County, dues have been reduced for 2026.
Speaking of membership, I want to recognize a few groups that have consistently shown outstanding support with 100% membership among physicians:
• West Reading Radiology – 28 (100%)
• Digestive Disease Associates – 21 (100%)

• Eye Consultants of PA – 13 (100%)
• Reading Pediatrics – 8 (100%)
• Center for Urologic Care – 7 (100%)
• Berks Eye Physicians and Surgeons – 6 (100%)
• Reading Nephrology – 6 (100%)
• Arthritis and Osteoporosis Center – 5 (100%)
• Berks Radiation Oncology Associates – 4 (100%)
• ENT Head and Neck Specialists – 4 (100%)
A big thank-you to these groups for their ongoing support of BCMS and commitment to our county. Many other groups and solo physicians also have 100% membership, but the editors wisely stopped me from turning this into a 500-page booklet of shout-outs.
As summer winds down and fall begins, take a moment to breathe and remember: what you do matters. No matter the national discourse, your work is vital to our community, our families, and our colleagues. Thank you, as always, for your dedication to our patients, our hospitals, and each other.

by D. Michael Baxter, MD Editor, the Medical Record
Lucy Cairns, MD Past-Editor, the Medical Record

While it is uncommon for two Editors to write their comments in our “Editor’s Notes” section, these are uncommon times. As the two of us worked together to publish this Fall edition, we were once again impressed by the dedication and enthusiasm of our summer research students, the Pat Sharma Berks County Medical Society Scholars, and the Reading Hospital Summer Interns. In their efforts, we are reminded of at least two hundred years of science-based research which has advanced the practice of medicine and nearly doubled our life expectancy. With the development of vaccines, antibiotics and the latest advancements in genetics and immunology, our investment in science has led the way to astonishing success.
This has been a relentless march of progress, until now. In recent months we have seen unprecedented attacks on multiple pillars of the U.S. health care and public health systems by many of those officials—especially at the federal level—who fund and control medical research and health policy. There have been crippling cuts in funding and staffing at the National Institutes of Health (NIH) and the Centers for Disease Control (CDC) and the disruption of the essential work of such voices of expertise as the Advisory Committee on Immunization Practices (ACIP), with recognized experts being fired and replaced with others of dubious experience with political agendas to expound. Very recently two of our largest organizations of medical professionals, the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians (AAFP), announced that they were rejecting certain vaccine guidelines by the CDC and making their own recommendations, an unprecedented move.
Simultaneously, some federal programs that fund health care and food security programs have been subject to major funding cuts and the tightening of eligibility criteria. These changes are predicted to result in large numbers of Americans losing their health

insurance and vital nutritional support. As the article in this issue by our local Helping Harvest community agency notes, this will have a significant negative impact on the lives of many people, our patients, in this community. The rise in the uninsured population from Medicaid cuts will have adverse consequences for the financial survival of hospitals and health systems, in addition to poorer health for the affected individuals.
Perhaps the most detrimental occurrence of all is the blatant attempt to undermine trust in the medical and public health professions by some who hold powerful positions in the federal government. Delegitimizing the work of established and respected experts in these fields opens the door to replacing the evidence-based approach to advancing healthcare and public health that has served our country well with one that serves a particular political ideology. The problem with allowing ideology to control healthcare decisions, rather than the best available evidence, is that outcomes are likely to miss the target we should all be aiming for, and do more harm than good. This should be unacceptable to a profession whose foundation depends on earning the trust of patients by putting their best interests above all.
At such times as this, one response would be to dismiss all of this and burrow deeper into our own work, doing the best we can with our own resources and abilities. However, if ever there was a time to stand for what we believe, for the oaths we have taken and the promises we have made to ourselves and to our patients, that time is now. There are avenues through our professional organizations and our elected representatives to demand accountability for truth and to ensure that fact-based science will guide our policy decisions and clinical choices. For over two hundred years this approach has led us to unimaginable advances in human health. Let us not now retreat.

Your new digital gateway to the latest WellSpan advances.
With articles, research updates and exclusive insights tailored for physicians, MacroScope is our new content platform to inform and inspire. We look forward to sharing medical innovations, clinical research and new technologies that will empower and inform your professional journey.
• Stay up to date: Keep abreast of the latest developments across various specialties.
• Gain insights: Benefit from expert analyses and studies that can directly impact your practice.
• Expand your network: Connect with other experts shaping the future of healthcare.
For another healthy dose of valuable medical content, subscribe to our companion publication. Complete the subscription form on MacroScope online for delivery to your home or office three times a year.

by Lucy J. Cairns, MD (retired)
The Pat Sharma President’s Scholarship Supporting the GenerationNext
In 2014 the Berks County Medical Society initiated a paid six-week summer program to provide local college students who have demonstrated an interest in medicine or public health with the opportunity to explore a topic of their choice under expert guidance, and to shadow clinicians in the office and operating room (OR). A cooperative relationship with the Reading Hospital’s Student Summer Internship has added greatly to the value of our program for the Pat Sharma scholars. This arrangement is currently enabled by Chief Academic Officer for Tower Health, Wei Du, MD. GME/UME Coordinators Ashley Morris and Sarah Saget do a superb job administering the hospital program and coordinating with our scholars.
Through this generous arrangement with Reading Hospital-Tower Health’s Academic Affairs team, our scholars are folded into the hospital program for the process of onboarding, have access to clinical shadowing and didactic sessions within the hospital, and join the hospital’s student interns in presenting their research work to a faculty panel at the end of the program. In turn, the BCMS is proud to
include abstracts submitted by the student researchers as a feature in this edition of the Medical Record. The variety and quality of the research being undertaken at Reading Hospital is reflected in these abstracts, which serve as a reminder of how fortunate we are to have in our community a medical institution focused on top-quality research and education, in addition to excellence in patient care.
Our community is also fortunate in the number of exceptionally capable young people who aspire to a career in medicine, looking to those of us who have gone before for encouragement and support. The applicants for the Pat Sharma President’s Scholarship appear more impressive with each passing year, presenting the selection committee with increasingly difficult choices.
Being able to offer a stipend to our scholars is a significant factor in attracting top applicants, made possible by the generous contributions of BCMS members to our Educational Trust. A large gift from retired vascular surgeon and past president of the BCMS, Pat Sharma, MD, in 2018 endowed this program with funds sufficient to support at least one student

per year. Another past president, retired neurosurgeon and current Medical Director of the Physicians Health Program of the Pennsylvania Medical Society Foundation, Raymond C. Truex Jr., MD, has supported additional Pat Sharma scholars in recent years, making the selection process a little less arduous. Our past and present scholars, and all the BCMS members who have found great reward in supporting this program through mentorships, owe Dr. Sharma and Dr. Truex a heartfelt debt of gratitude.
The 2025 Pat Sharma scholars are Cyrus Rahmanian and Emily Shirk. Cyrus graduated this year from Elizabethtown College in Lancaster, PA, with a major in Public Health. As an undergraduate student, among other achievements, Cyrus developed an interactive map using a Geographic Information System (GIS) displaying all U.S. thoracic transplant centers and their academic affiliation. This was designed for transplant teams to identify institutions capable of treating transplant patients who travel or relocate. With this mapping tool he also identified rural areas lacking adequate access to transplant services. Cyrus is currently a
student in a post-BA program at Drexel University that provides a pathway to medical school. He aspires to work in the field of transplant medicine and develop an effective treatment for chronic organ rejection.
Emily Shirk is completing her senior year as a biology major, with minors in public health and philosophy, at Drew University in Madison, NJ. In the 20212022 school year, Emily earned a 4.0 GPA in the Medical Health Professions Program through Berks Career & Technology Center, Penn State Berks, and Tower Health. In May of this year, she helped provide medical care to under-resourced communities in Panama with the Global Medical Brigade. Emily is strongly motivated by a desire to help shape the future of healthcare, possibly in a primary care role.
Emily and Cyrus were able to delve into topics of special interest to them—very complex topics—and produce research papers illustrating a good grasp of the subject thanks to close mentoring by BCMS members. Dr. Shoja S. Rahimian, a Medical Oncologist with the McGlinn Cancer Institute – Reading Hospital, guided Cyrus through his examination of the outcomes of Solid Organ Transplant Patients treated for cancer with immune checkpoint inhibitor drugs. Emily’s analysis of the evidence for connections between anxiety disorders and dysbiosis in the gut, and the intervention strategies that might be developed based on braingut microbiome interactions, was carried out with the generous aid of Dr. Eduardo Espiridion, Chair of the Department of Psychiatry at Reading Hospital-Tower Health, and Anna (Marianna) Bluestone, Registered Dietician with Reading Hospital. These clinicians repeatedly made time in their busy days to share their expertise with Emily and Cyrus.
The willingness of a long list of physicians, both within the Tower Health System and in independent practice, to allow our students to spend time shadowing them in the clinic and OR also contributes hugely to the value students
A New Face with a Clear Vision

Eye Consultants of Pennsylvania is excited to welcome Tianyu (Tom) Liu, MD, an award-winning, board-certified retinal specialist. Dr. Liu is fellowship-trained in vitreoretinal surgery and offers advanced care for conditions such as retinal detachments, diabetic retinopathy, and age-related macular degeneration. A graduate of the University of Pennsylvania’s Perelman School of Medicine, Dr. Liu has earned numerous national honors and trained at some of the most respected programs in the country.
Whether you’re facing a complex retinal condition or seeking expert guidance on your eye health, you can trust Dr. Liu to provide compassionate, personalized care to protect and preserve your vision.
NOW ACCEPTING NEW PATIENTS AND PHYSICIAN REFERRALS IN WYOMISSING AND POTTSVILLE
Call 1-800-762-7132 or visit eyeconsultantsofpa.com today!
find in the Pat Sharma program. There is no replacement for the experience of oneon-one time with medical professionals for college students contemplating a career in healthcare. Space does not allow mention of the names of all these outstanding members of our Berks County medical community, but please know that you are much appreciated. The ongoing success of
the Pat Sharma President’s Scholarship is the result of a combined effort, and any BCMS member who would like to contribute financially or volunteer as a mentor is urged to join those of us who find this project invariably rewarding by contacting our Executive Director, Beth Gerber, at bgerber@ berkscms.org.



Outcomes in Solid Organ Transplant Patients Receiving Immune Checkpoint Inhibitors
Lucy J. Cairns, MD, Berks County Medical Society
INTRODUCTION
Immune checkpoint inhibitors (ICI) as a form of immunotherapy have changed the standards of cancer care in numerous indications. By targeting pathways in T-cells to enhance anti-tumor responses, ICIs have shown significant efficacy (Doroshow 2021). It is estimated that 44% of newly diagnosed cancer patients are eligible for ICIs (Haslam, 2025). Cancer is the second leading cause of death in transplant patients (Saleem, 2025).
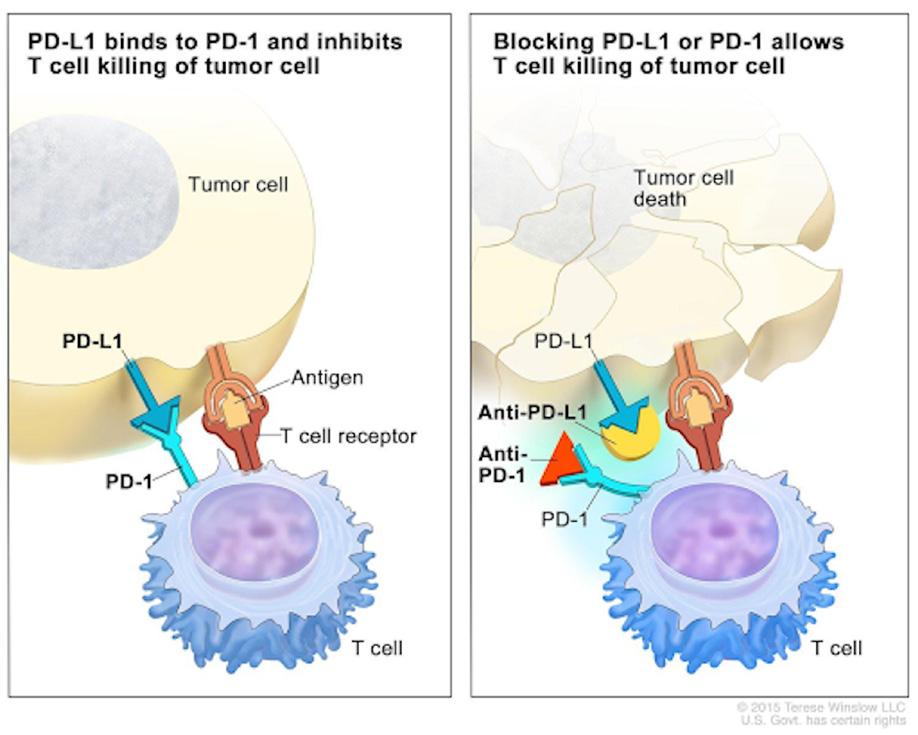
Among the most common ICIs are programmed cell death-ligand (PD-L1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). Common ICIs targeting the PD-1 receptor are nivolumab, pembrolizumab, and cemiplimab. Common PD-L1 inhibitors include atezolizumab, avelumab, and durvalumab. Tumor cells can express the PD-L1 protein, which binds to the PD-1 receptor to negatively regulate the T-cell and prevent it from attacking the tumor cell (Figure 1, NCI Winslow, 2022). ICI therapy blocks this interaction, allowing the T-cell to recognize and attack the tumor cell.
ICI as a cancer treatment modality, however, presents concerns when treating transplant patients who are on immunosuppressants to stop T-cell mediated rejection. T-cells are the main cause of allograft rejection in transplant patients, due to allorecognition of foreign antigens causing the T-cells to attack the transplanted organ

(Issa, 2010). Immune checkpoint inhibitors can inadvertently activate the body’s immune response towards T-cell mediated lysis of graft cells in the transplanted organ, similar to acute allograft rejection (Justiz, 2024). Most commonly, this can present challenges for kidney transplant patients, who represent the largest population in solid organ transplants. This paper explores the potential challenges of using immune checkpoint inhibitors in solid organ transplant recipients with cancer and highlights clinical outcomes and future directions in the field of immunology for this population.
TRANSPLANT IMMUNOLOGY
To reduce the risk of allograft rejection, Solid Organ Transplant Recipients (SOTR) take medication to suppress their immune system. A rejection episode occurs when the patient’s own body is producing T-cells that recognize the donor organ as foreign and start attacking it, which can lead to organ failure. The two most common types of rejection found in SOTR are acute rejection and chronic rejection. Acute rejection typically occurs within days or months after the transplantation and involves the body recognizing the donor organ as foreign in a T-cell mediated response. This form of rejection is the most common in SOTR, with an incidence rate of 50% to 70% within the first few months of the transplant (Justiz, 2024). Acute rejection is commonly treated with steroids (Murakami, 2021). Chronic rejection can occur further down the road, including months or years after transplantation. This form of
rejection involves inflammation and an immune response against the transplanted organ. Chronic rejection can be managed by immunosuppressants, but there is currently no cure and it is not fully understood (Justiz, 2024).
KIDNEY TRANSPLANT RECIPIENTS
Kidney transplant Patients Receiving Immune Checkpoint Inhibitors
A multicenter study was conducted between 2010 and 2020 across 23 institutions involving kidney transplant recipients receiving ICI. There were 69 participants in this retrospective cohort study receiving immunotherapy for cancer. The most common cancers in the cohort were squamous cell carcinoma, with 24 cases, and melanoma with 22 (Murakami, 2021). After the 69 patients received immunotherapy, 29 of them developed acute rejection. Sixteen of the 29 patients who developed acute rejection were treated with high dose intravenous corticosteroids. Forty-five of the patients changed their immunosuppressive medication prior to starting immunotherapy and the most common change was from CNI to mTORi, making up 15 of the 45 changes (Murakami). Fourteen patients also increased their corticosteroids. Fourteen of the 29 patients with acute rejection were on pembrolizumab, a PD-1 inhibitor. One of the 29 patients was on ipilimumab, a CTLA-4 inhibitor, and 6 patients were on a combination of PD-1/CTLA4 regimens (Murakami, 2021). Anti-CTLA-4 immunotherapy resulted in a higher risk of allograft rejection compared to anti PD-L1.
Kidney Transplant Patients Not Receiving Immune Checkpoint
Inhibitors
There were 37 transplant patients who underwent treatment for cancer who did not receive immunotherapy. The most common cancers in this cohort were squamous cell carcinoma, with 23 cases, and melanoma with 14. Twenty of the 23 patients with cSCC received systemic cancer-directed therapy. Twelve of those 20 patients received cetuximab.
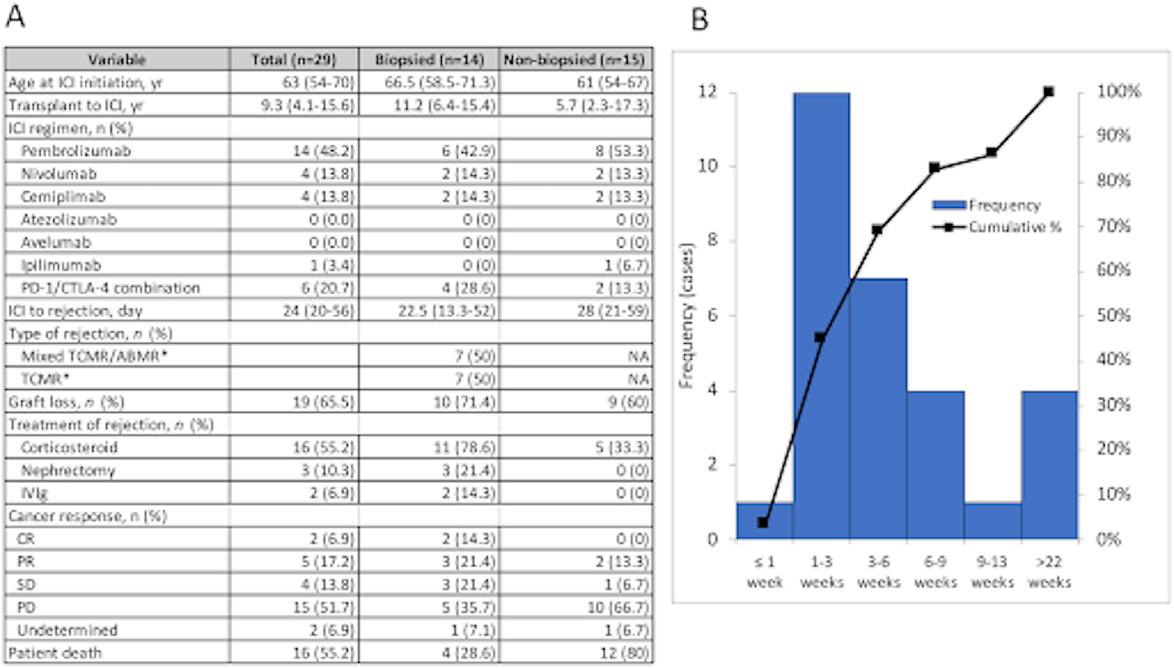
Melanoma Cohort
The 22 patients receiving ICI who were diagnosed with melanoma had a graft rejection rate of 54.5% compared to 7.1% in the non ICI group (n=14) p<0.01 (Murakami, 2021). The response rate of the cancer to ICI was 40.0%. One patient had a complete response to the immunotherapy and 7 had partial responses. One achieved stable disease, and 11 patients had progressive disease. Eleven of the patients were treated with pembrolizumab and 8 were treated with a combination therapy.
Squamous Cell Carcinoma Cohort
There were 24 patients who received ICI and 23 non-ICI treatment for cSCC. The rejection rate was much greater in the ICI group with 9 (37.5%) of the patients developing rejection compared to just 1 (4.3%) patient in the non-ICI group. The tumors of 2 patients on ICI had a complete response to the treatment and 6 had a partial response. Ten (41.7%) patients in the ICI group had progressive disease while 18 (78.3%) in the non-ICI group had progressive disease.
LUNG & HEART TRANSPLANT RECIPIENTS
An analysis of 140 studies involving SOTR receiving ICIs included 343 transplant patients receiving ICIs. Among the 343 were 5 lung transplant patients and 18 heart transplant patients. The study concluded that 2 (40%) of the lung transplant patients experienced graft rejection and 7 (38.9%) of heart transplant patients receiving ICIs had graft rejection (Saleem, 2025).
Patient Response
Of the 343 patients on ICI, 116 (33.8%) of them developed rejection. Sixty-nine (59.5%) of those patients experienced rejectioninduced graft loss (Saleem, 2025). The tumor responses (n=303) for patients were the following: 49 (16.2%) had complete response, 65 (21.5%) had partial response, 48 (15.8%) had stable disease, continued on next page >
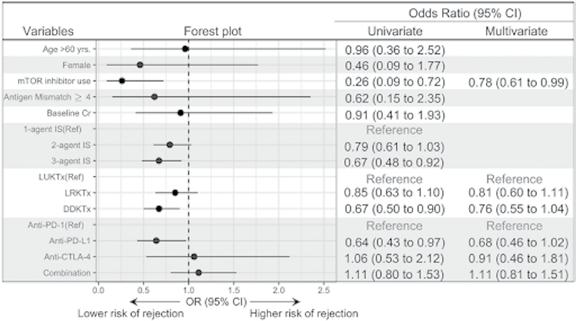

and 138 (45.5%) had progressive disease. Fifty-three patients were surveyed on their quality of life after receiving ICIs. Twenty-six (49%) said their quality of life improved while 27 (51%) said their quality of life worsened.
OUTCOMES
Forty-two percent of kidney transplant patients developed acute rejection, 65% of whom did not recover and had graft loss and needed dialysis. While treatment with ICIs is associated with high acute rejection rates, it also appears to improve the odds of a positive tumor response. Five of the patients on an ICI had a complete response to the treatment, 15 had a partial response, and 11 had stable disease, for a total of 31 patients experiencing a positive tumor response to the immune checkpoint inhibitor treatment for their cancer. Thirty-four (49.3%) of the patients treated with an ICI experienced progressive disease, compared with 28 (75.7%) of those not treated with an ICI. This shows that ICI treatment increases the odds of a positive response when used to treat cancer in transplant patients. Unfortunately, it also increases the risk of acute rejection. The transplant patient group which did not receive ICIs had an acute rejection rate of just 5.4%, compared to a 42% acute rejection rate in the ICI-treated group (Murakami, 2021).
TREATMENT CONSIDERATIONS
The average time from transplantation of the donor kidney to ICI treatment was 9 years in the cohort study (Murakami, 2021). The average time from transplant to diagnosis was 12 years for cSCC and 7.7 years for melanoma. The average life expectancy of a kidney transplant recipient can vary due to numerous reasons, such as whether the organ was a living donor kidney (15-20 years) or deceased donor kidney (10-15 year years). While immune checkpoint inhibitors appear to be an effective cancer treatment, their use in SOTR patients greatly increases the risk of developing acute rejection. It is important to have discussions between the patient’s multidisciplinary care teams and the patient to decide if treatment with ICI is worth pursuing to treat their cancer. It is important to note that transplant patients with cancer are not eligible for a re-transplant if they still have cancer, a reality which may affect the decision making on whether to use ICI or not. It is also important to consider which organ is transplanted, as there is no long-term option for managing lung failure or heart failure, while there are options like dialysis for kidney patients who have graft-induced organ failure. Physicians may be more inclined to aggressively treat a cancer with ICI in a patient with a transplanted kidney, knowing that they can go on dialysis if there is organ failure.
DISCUSSION
Immune checkpoint inhibitors are an effective treatment for attacking cancer, but their use also results in a high risk of rejection among transplant patients. This raises ethical concerns with care teams as they attempt to balance the risk vs reward. There are hundreds of known biomarkers, and new ones being discovered, which may lead to new treatments being developed that may include safer options for transplant patients. (Chronic rejection still has no cure, and it may be worthwhile to look into the use of the PD-1 and PD-L1 mechanism in donor organs to combat T-cell mediated rejection.) At the end of the day, the decision is up to the patient. Care teams can educate the patient using these studies and strategize to mitigate the risk of rejection and adjust the patient’s immunosuppressive regimen.

References
Carlino, M. S., Larkin, J., & Long, G. V. (2021). Immune checkpoint inhibitors in melanoma. Lancet (London, England), 398(10304), 1002–1014. https://doi.org/10.1016/S0140-6736(21)01206-X
Doroshow, D. B., Bhalla, S., Beasley, M. B., Sholl, L. M., Kerr, K. M., Gnjatic, S., Wistuba, I. I., Rimm, D. L., Tsao, M. S., & Hirsch, F. R. (2021). PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nature reviews. Clinical oncology, 18(6), 345–362. https://doi.org/10.1038/s41571-02100473-5
Issa, F., Schiopu, A., & Wood, K. J. (2010). Role of T cells in graft rejection and transplantation tolerance. Expert review of clinical immunology, 6(1), 155–169. https://doi.org/10.1586/eci.09.64

Murakami, N., Mulvaney, P., Danesh, M., Abudayyeh, A., Diab, A., Abdel-Wahab, N., Abdelrahim, M., Khairallah, P., Shirazian, S., Kukla, A., Owoyemi, I. O., Alhamad, T., Husami, S., Menon, M., Santeusanio, A., Blosser, C. D., Zuniga, S. C., Soler, M. J., Moreso, F., Mithani, Z., … Immune Checkpoint Inhibitors in Solid Organ Transplant Consortium (2021). A multi-center study on safety and efficacy of immune checkpoint inhibitors in cancer patients with kidney transplant. Kidney international, 100(1), 196–205. https://doi.org/10.1016/j.kint.2020.12.015
Naimi, A., Mohammed, R. N., Raji, A., Chupradit, S., Yumashev, A. V., Suksatan, W., Shalaby, M. N., Thangavelu, L., Kamrava, S., Shomali, N., Sohrabi, A. D., Adili, A., Noroozi-Aghideh, A., & Razeghian, E. (2022). Tumor immunotherapies by immune checkpoint inhibitors (ICIs); the pros and cons. Cell communication and signaling : CCS, 20(1), 44. https://doi. org/10.1186/s12964-022-00854-y
Nguyen, L. S., Ortuno, S., Lebrun-Vignes, B., Johnson, D. B., Moslehi, J. J., Hertig, A., & Salem, J. E. (2021). Transplant rejections associated with immune checkpoint inhibitors: A pharmacovigilance study and systematic literature review. European journal of cancer (Oxford, England : 1990), 148, 36–47. https://doi.org/10.1016/j.ejca.2021.01.038
Saleem, N., Wang, J., Rejuso, A., Teixeira-Pinto, A., Stephens, J., Wilson, A., Kieu, A., Gately, R., Boroumand, F., Chung, E., Bonevski, B., Carlino, M., Carroll, R., Lim, W., Craig, J., Murakami, N., & Wong, G. (2025). Outcomes of Solid Organ Transplant Recipients With Advanced Cancers Receiving Immune Checkpoint Inhibitors. JA
Simon, S., & Labarriere, N. (2017). PD-1 expression on tumor-specific T cells: Friend or foe for immunotherapy?. Oncoimmunology, 7(1), e1364828. https://doi.org/10.1080/2162402X.2017.1364828
Tabrizian, P., Abdelrahim, M., & Schwartz, M. (2024). Immunotherapy and transplantation for hepatocellular carcinoma. Journal of hepatology, 80(5), 822–825. https://doi.org/10.1016/j.jhep.2024.01.011
Tang, Q., Chen, Y., Li, X., Long, S., Shi, Y., Yu, Y., Wu, W., Han, L., & Wang, S. (2022). The role of PD-1/PD-L1 and application of immunecheckpoint inhibitors in human cancers. Frontiers in immunology, 13, 964442. https://doi.org/10.3389/fimmu.2022.964442
Tejani, A., & Emmett, L. (2001). Acute and chronic rejection. Seminars in nephrology, 21(5), 498–507. https://doi.org/10.1053/snep.2001.24945
Vera, R. (no date) WCN24-1341 prevalence of rejection in kidney transplant patients at the Hospital de Clínicas - Kidney International Reports. Available at: https://www.kireports.org/article/S2468-0249(24)01059-3/fulltext


Specializing in the diagnosis and treatment of ALL neck and back disorders.
ALL SURGERY PERFORMED IN BERKS COUNTY
• Pain Management
• Physical Therapy
• Epidural Injections
• Spinal Surgery
2607 Keiser Blvd, Suite 200, Wyomissing, PA 19610 484-509-0840







Evidence for Association, Gut-Brain Axis Mechanisms, and Intervention Strategies
BCMS Pat Sharma President’s Scholarship Recipient
Preceptors: Eduardo D. Espiridion, MD, Chair, Dept. of Psychiatry, Reading Hospital/Tower Health
Marianna Bluestone, Registered Dietician
Eve Kimball, MD, FAAP
INTRODUCTION:
Approximately one in five adults in the United States experience symptoms of an anxiety disorder (28). Characterized by excessive worrying and anxious thoughts that do not subside, an anxiety disorder can be debilitating and interfere with normal social and occupational life. The cause of anxiety is not well understood. Genetics, brain chemistry, and environmental stress may all play a role in the development of this psychiatric disorder (29). In recent years, research exploring the various connections between the brain and gut, also known as the gut-brain axis, has illustrated a potential link between the resident microorganisms in the large intestine and the host’s mental health (6). The microbiomegut-brain axis refers to the two-way communication between the gut microflora and the brain via neuronal signaling, hormones, chemical messengers, and the immune system. A condition that elucidates this connection well is irritable bowel syndrome (IBS). Patients with IBS are 3 times more likely to have anxiety compared to healthy individuals, highlighting that abnormalities in the gut may impact mental health; however, this relationship is not well understood (26). The aim of this article is to examine the relationship between gut microbiota composition and anxiety, explore some possible mechanisms that may contribute to this relationship, and evaluate possible gut interventions as a means to improve anxiety symptoms.

GUT MICROBIOME
By definition, the gut microbiome refers to the collection of bacteria and other microorganisms that inhabit the gastrointestinal tract, spanning from mouth to anus. However, when people refer to the “gut microbiome,” they are often referencing the bacterial species residing in the colon, which contains approximately 70% of the body’s total microbial population (16). The dominant phyla of the colon are Firmicutes (Gram-positive) and Bacteroidetes (Gram-negative). These bacteria have a commensal relationship with their human host, meaning that they benefit from living in the rich environment of the colon, and the human host simultaneously benefits from their activity.
The primary role of a healthy gut microbiome is to break down carbohydrates that are indigestible to the host, also known as soluble fiber, to produce short-chain fatty acids (SCFAs). Gut bacteria can also break down proteins, produce vitamins K and B, and metabolize drugs and other foreign substances. The gut microbiome also plays an integral role in immune regulation by outcompeting pathogenic bacteria and stimulating immune responses of host cells to prevent pathogenic colonization. Finally, a healthy gut microbiome is also responsible for maintaining the integrity of the gut barrier by promoting tight epithelial junctions, preventing host epithelial cell loss, and modulating host signaling

Dysbiosis refers to a disturbance in the microbial equilibrium due to an imbalance of flora, changes in flora metabolism, or changes in their spatial distribution (8). Dysbiosis can involve a loss of beneficial organisms, a growth of harmful organisms, and/or an overall loss of microbial diversity. In addition to IBS, scientists have also found connections between dysbiosis and obesity, allergies, Type 1 diabetes, autism, and colorectal cancer.
DYSBIOSIS AND ANXIETY
Multiple studies have shown that people with anxiety tend to have a different microbiota composition compared to those without anxiety. A 2025 systematic review of 8 cross-sectional studies analyzing human fecal samples found that the gut microbiome of patients with diagnosed anxiety disorders was significantly different from that of healthy controls. Decreases in Faecalibacterium, Coprococcus, and Eubacterium were observed, all of which are genera within the Firmicutes phylum. Furthermore, in some studies, individuals who were actively experiencing anxiety symptoms had lower levels of Faecalibacterium compared to those who had recovered from anxiety disorders, suggesting that the microbiome may shift alongside changes in mental health. Patients with generalized anxiety disorder were also reported to have increased levels of Bacteroides, Ruminococcus gnavus, and Fusobacterium (2) .
Another cross-sectional study conducted on gastrointestinal clinic patients found significant differences in the microbiome based on levels of anxiety. Similar to the 2025 study, the researchers found that patients who scored higher on anxiety scales had less Faecalibacterium and Bifidobacterium. Bifidobacterium belongs in the phyla Actinobacteria, which was, in general, less represented in anxious microbiomes. Anxious patients also showed a greater abundance of Clostridioides and Bacteroides (14)
POSSIBLE MECHANISMS
There are a variety of gut-brain axis mechanisms that may explain microbiota imbalances manifesting as anxiety symptoms. Faecalibacterium, Coprococcus, and Eubacterium, all genera shown to be depleted in anxious patients across multiple studies, are major SCFA-producers within the gut, specifically of butyrate (20, 25, 22) . SCFAs within the gut have many beneficial properties, including induction of enteric serotonin production and maintenance of tight junctions. These properties of SCFAs may help to explain the relationship between dysbiosis and anxiety. Animal models have shown that supplementation with SCFAs helps to reduce anxiety symptoms in response to psychosocial stressors; however, this has not been shown in humans yet (30) .
Within the gut, SCFAs stimulate specialized host cells called enterochromaffin (EC) cells, which are responsible for producing 90-95% of the body’s serotonin. In a two-step enzymatic reaction, EC cells convert tryptophan into serotonin using the enzymes tryptophan hydroxylase 1 (TPH1) and aromatic L-amino acid decarboxylase (19). Mouse studies have shown that the gut microbiome is essential for serotonin synthesis, as germ-free mice, continued on next page >




Do you have patients with:
• Chronic Headaches
• Tinnitus
• Jaw Pain
• Insomnia
• Ear Pain without signs of infection
• Dizziness
• Clicking, popping, or grating in the jaw joint
• Limited jaw opening or locking
• Swallowing difficulty
• Snoring
• Pain when chewing
• Sleep issues
• Facial pain
• Neck pain or stiffness
• Tired jaws
• CPAP Intolerance
If so, they may be suffering from TMJ Dysfunction and/or Sleep Disordered Breathing, such as snoring and obstructive sleep apnea. We offer comprehensive diagnosis and treatment. Our many years of experience have resulted in a high rate of successful outcomes.
Our philosophy involves a conservative, non-surgical, non-pharmaceutical approach to management with an emphasis on multidisciplinary care.




or mice lacking any microbiome, exhibit significantly reduced TPH1 expression in the colon, indicating impaired serotonin production. These germ-free mice also displayed increased anxietylike behaviors (24). Enteric serotonin acts on the vagus nerve, which is the main nerve connecting the gut to the brain (15). In a study looking at anxious and depressive behaviors of mice based on their gut microbiota, the patterns studied were not seen when the mouse’s vagus nerve was cut, showing that many anti-anxiety properties of the gut-microbiota are vagus nerve-dependent (5). Vagus nerve activity has anti-anxiety effects: it activates the parasympathetic nervous system and suppresses the hypothalamic pituitary axis (HPA), which is associated with cortisol release (23). Overall, a lack of SCFA-producing bacteria could lead to anxiety via decreased SCFAinduced vagus nerve activity.
In addition to depletion of serotonin, a lack of SCFAs due to dysbiosis may also lead to increased free tryptophan. Tryptophan that is not converted into serotonin can be metabolized through the kynurenine pathway, and since both serotonin and kynurenine are derived from the same precursor—tryptophan—it is plausible that decreased SCFAs and associated decreased serotonin production could push tryptophan down the kynurenine pathway (10). Similarly, butyrate, which may be depleted in anxious patients, suppresses the enzyme that converts tryptophan into kynurenine, indoleamine 2,3-dioxygenase (IDO) (21). This may also explain the beneficial role of SCFAs on serotonin production. In a study of social anxiety disorder, subjects with anxiety had significant alterations in their tryptophan-kynurenine pathway (3). Researchers suggest that KYNA, a metabolite of kynurenine that was higher in anxious patients, may impact glutamate signaling, resulting in anxiety. Other research suggests that quinolinic acid, another metabolite of kynurenine, is also associated with anxiety (18). The combination of decreased serotonin and increased neuroactive kynurenine metabolites may both contribute to worsened host mental health.
Butyrate and other SCFAs also help to maintain the tight junctions between gut epithelial cells. Animal models have shown that germ-free mice have increased intestinal permeability; however, this permeability could be reversed with supplementation of SCFAs and SCFA-producing bacteria (4). Increased permeability of the gut epithelium allows gut microbiota and bacterial products, like lipopolysaccharide (LPS), to enter the bloodstream, causing cytokine production and low-grade inflammation. Additionally, some research suggests that LPS may directly contribute to gut permeability (7). It is important to note that some species that were particularly high in anxious people, like Bacteroides and Fusobacterium, produce LPS, which could contribute to more inflammation. These inflammatory cytokines can act locally, similar to serotonin, or unlike serotonin, they can cross the blood-brain barrier and act directly on neurons in the brain (13). Low-grade inflammation and elevated cytokine levels are associated with increased anxiety by disrupting neurotransmitter systems, activating microglia, and impairing brain circuits involved in emotional regulation (13). This condition is more commonly referred to as “leaky gut.” A 2018 study found correlations between anxiety and circulating LPS, as well as Zonulin and FABP2, two proteins that indicate leaky gut syndrome in subjects that did not have gastrointestinal disorders (27). This shows that anxious patients may be experiencing “leaky gut” without the common accompanying gastrointestinal disorders. Additionally, inflammatory cytokines activate IDO which may also contribute to anxious symptoms via the tryptophan-kynurenine pathway (18) .
Various other pathways of the microbiome gut-brain axis may explain connections to anxiety, including GABA, hydrogen sulfide, and other immune functions; however, due to the scope of this article, they are not discussed here (6)


Connecting Berks County to Addiction Resources
Local Treatment and Recovery Resources
Free NARCAN Kits
Free Medication Lock Boxes
Community and School Education
Free Tobacco Cessation Classes
INTERVENTIONS
Treatment of dysbiosis often involves probiotics, prebiotics, and diets high in fiber. Understanding these treatments as a means to mitigate anxiety symptoms could be beneficial for many patients, as dietary changes and pre- and probiotic supplements tend to have less negative side effects than conventional anxiety treatments such as serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) (11) .
Unfortunately, the species that are depleted in anxious patients, such as Faecalibacterium, Eubacterium, and Coprococcus, are challenging to culture into probiotics, as they are obligate anaerobes and sensitive to oxygen (20, 25, 22). There is ongoing research to develop “next-generation” probiotics by culturing butyrate-producing anaerobic bacteria, such as Faecalibacterium, in combination with sulfate-reducing bacteria. However, this work is still in early stages and has not yet led to commercially available products (17)
Consuming more dietary fiber could be a way to increase SCFAs and SCFA-producing bacteria to alleviate dysbiosis related to anxiety. While limited research is currently available on the relationship between high dietary fiber intake and anxiety, there are a few promising cross-sectional studies that together reveal a significant inverse relationship between fiber consumption and . Fiber intake in this meta-analysis was based on
(610) 376-8669 cocaberks.org

fiber supplementation and self-reported diet. However, at this time no randomized controlled trials have shown that fiber consumption can be an efficacious treatment for anxiety. Prebiotics, a specific type of fermentable fiber, have also been associated with improved anxiety symptoms. A randomized controlled trial has shown that a diet naturally rich in prebiotic fibers may support mood, reduce anxiety and stress, and improve sleep in adults, while probiotic supplements or combinations of pre- and probiotics did not show the same effect (9). This shows that dietary changes tend to be more impactful than supplements. More research, specifically randomized controlled trials, should be conducted to study the impact of dietary fiber intake, probiotics, and prebiotics, as these treatments have far less negative symptoms compared to conventional anti-anxiety medications.
CONCLUSION
This review aimed to explore the relationship between dysbiosis and anxiety, potential pathways of the gut-brain axis, and interventions. Anxious patients tended to have decreased Faecalibacterium, Eubacterium, and Coprococcus and increased Bacteroides and Fusobacterium. Potential pathways explaining this association involving reduced SCFAs, decreased enteric serotonin, increased kynurenine metabolites, decreased vagus nerve stimulation, continued on next page >
and inflammation were not linear. Increased dietary fiber and prebiotics may show promise for alleviating anxiety.
While some preliminary research has shown a connection between dysbiosis and anxiety, and some proposed mechanisms have been explained above, it is important to note that the dysbiosis may not be a cause of anxiety but rather an effect. The gut-brain axis is a bidirectional pathway in which the gut is also influenced by the brain, which was not explored in this paper. Many studies show that even very small and short-lasting stressors can change microbial concentrations (12). The association between dysbiosis and anxiety is important to explore further, as definitive and direct pathways have yet to be determined. Additionally, the research that has been cited may be limited by small sample sizes or animal models. Larger-scale cross-sectional and experimental studies of humans should be conducted in order to better understand this convoluted relationship. The gut-brain axis is a fascinating topic with many facets that have yet to be explored, but with more research scientists may be able to find efficacious and low-risk treatments for anxiety disorders.

Emily Shirk is a senior at Drew University in Madison, New Jersey. Her major field of study is Biology with minors in Public Health and Philosophy. Her career plan is to apply to medical school.
References
1. Aslam, H., Lotfaliany, M., So, D., Berding, K., Berk, M., Rocks, T., Hockey, M., Jacka, F. N., Marx, W., Cryan, J. F., & Staudacher, H. M. (2024). Fiber intake and fiber intervention in depression and anxiety: a systematic review and meta-analysis of observational studies and randomized controlled trials. Nutrition reviews, 82(12), 1678–1695. https://doi.org/10.1093/nutrit/ nuad143
2. Butler, M. I., Kittel-Schneider, S., Wagner-Skacel, J., Mörkl, S., & Clarke, G. (2025). The Gut Microbiome in Anxiety Disorders. Current psychiatry reports, 27(5), 347–361. https://doi.org/10.1007/s11920-025-01604-w
3. Butler, M. I., Long-Smith, C., Moloney, G. M., Morkl, S., O’Mahony, S. M., Cryan, J. F., Clarke, G., & Dinan, T. G. (2022). The immune-kynurenine pathway in social anxiety disorder. Brain, behavior, and immunity, 99, 317–326. https://doi.org/10.1016/j.bbi.2021.10.020
4. Braniste, V., Al-Asmakh, M., Kowal, C., Anuar, F., Abbaspour, A., Tóth, M., Korecka, A., Bakocevic, N., Ng, L. G., Kundu, P., Gulyás, B., Halldin, C., Hultenby, K., Nilsson, H., Hebert, H., Volpe, B. T., Diamond, B., & Pettersson, S. (2014). The gut microbiota influences blood-brain barrier permeability in mice. Science translational medicine, 6(263), 263ra158. https://doi. org/10.1126/scitranslmed.3009759
5. Bravo, J. A., Forsythe, P., Chew, M. V., Escaravage, E., Savignac, H. M., Dinan, T. G., Bienenstock, J., & Cryan, J. F. (2011). Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences of the United States of America, 108(38), 16050–16055. https://doi.org/10.1073/ pnas.1102999108

6. Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gutbrain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of gastroenterology, 28(2), 203–209. https://pmc.ncbi.nlm.nih. gov/articles/PMC4367209/
7. Chelakkot, C., Ghim, J. & Ryu, S.H. Mechanisms regulating intestinal barrier integrity and its pathological implications. Exp Mol Med 50, 1–9 (2018). https://doi.org/10.1038/s12276-018-0126-x
8. DeGruttola, A. K., Low, D., Mizoguchi, A., & Mizoguchi, E. (2016). Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflammatory bowel diseases, 22(5), 1137–1150. https://doi.org/10.1097/ MIB.0000000000000750
9. Freijy, T. M., Cribb, L., Oliver, G., Metri, N.-J., Opie, R. S., Jacka, F. N., Hawrelak, J. A., Rucklidge, J. J., Ng, C. H., & Sarris, J. (2023). Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health: The “Gut Feelings” randomised controlled trial. Frontiers in Neuroscience, 16, 1097278. https://doi.org/10.3389/fnins.2022.1097278
10.Gao, K., Mu, C. L., Farzi, A., & Zhu, W. Y. (2020). Tryptophan Metabolism: A Link Between the Gut Microbiota and Brain. Advances in nutrition (Bethesda, Md.), 11(3), 709–723. https://doi.org/10.1093/advances/ nmz127
11. Garakani, A., Murrough, J. W., Freire, R. C., Thom, R. P., Larkin, K., Buono, F. D., & Iosifescu, D. V. (2020). Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment Options. Frontiers in psychiatry, 11, 595584. https://doi.org/10.3389/fpsyt.2020.595584
12. Geng, S., Yang, L., Cheng, F., Zhang, Z., Li, J., Liu, W., Li, Y., Chen, Y., Bao, Y., Chen, L., Fei, Z., Li, X., Hou, J., Lin, Y., Liu, Z., Zhang, S., Wang, H., Zhang, Q., Wang, H., Wang, X., … Zhang, J. (2020). Gut Microbiota Are Associated With Psychological Stress-Induced Defections in Intestinal and BloodBrain Barriers. Frontiers in microbiology, 10, 3067. https://doi.org/10.3389/ fmicb.2019.03067
13. Guo, B., Zhang, M., Hao, W. et al. Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry 13, 5 (2023). https://doi.org/10.1038/s41398-022-02297-y
14. Hazan, S., von Guttenberg, M., Vidal, A. C., Spivak, N. M., & Bystritsky, A. (2024). A Convenience Sample Looking at Microbiome Differences Between Anxious and Non-Anxious Patients in a GI Clinic. Gastroenterology Insights, 15(4), 1054-1063. https://doi.org/10.3390/gastroent15040072
15. Hwang, Y. K., & Oh, J. S. (2025). Interaction of the Vagus Nerve and Serotonin in the Gut-Brain Axis. International journal of molecular sciences, 26(3), 1160. https://doi.org/10.3390/ijms26031160
16. Jandhyala, S. M., Talukdar, R., Subramanyam, C., Vuyyuru, H., Sasikala, M., & Nageshwar Reddy, D. (2015). Role of the normal gut microbiota. World journal of gastroenterology, 21(29), 8787–8803. https://doi.org/10.3748/wjg. v21.i29.8787
17. Khan, M. T., Duncan, S. H., Stams, A. J. M., van Dijl, J. M., Flint, H. J., & Harmsen, H. J. M. (2023). Synergy and oxygen adaptation for development of next-generation probiotics. Nature, 619(7972), 743–750. https://doi. org/10.1038/s41586-023-06378-w
18. Kim, Y. K., & Jeon, S. W. (2018). Neuroinflammation and the ImmuneKynurenine Pathway in Anxiety Disorders. Current neuropharmacology, 16(5), 574–582. https://doi.org/10.2174/1570159X15666170913110426
19. Liu, N., Sun, S., Wang, P., Sun, Y., Hu, Q., & Wang, X. (2021). The Mechanism of Secretion and Metabolism of Gut-Derived 5-Hydroxytryptamine. International Journal of Molecular Sciences, 22(15), 7931. https://doi. org/10.3390/ijms22157931

20. Martín, R., Rios-Covian, D., Huillet, E., Auger, S., Khazaal, S., Bermúdez-Humarán, L. G., Sokol, H., Chatel, J. M., & Langella, P. (2023). Faecalibacterium: a bacterial genus with promising human health applications. FEMS microbiology reviews, 47(4), fuad039. https://doi.org/10.1093/femsre/ fuad039
21. Martin-Gallausiaux, C., Larraufie, P., Jarry, A., Béguet-Crespel, F., Marinelli, L., Ledue, F., Reimann, F., Blottière, H. M., & Lapaque, N. (2018). Butyrate Produced by Commensal Bacteria Down-Regulates Indolamine 2,3-Dioxygenase 1 (IDO-1) Expression via a Dual Mechanism in Human Intestinal Epithelial Cells. Frontiers in immunology, 9, 2838. https:// doi.org/10.3389/fimmu.2018.02838
22. Notting, F., Pirovano, W., Sybesma, W., & Kort, R. (2023). The butyrateproducing and spore-forming bacterial genus Coprococcus as a potential biomarker for neurological disorders. Gut microbiome (Cambridge, England), 4, e16. https://doi.org/10.1017/gmb.2023.14
23. Richer, R., Zenkner, J., Küderle, A., Rohleder, N., & Eskofier, B. M. (2022). Vagus activation by Cold Face Test reduces acute psychosocial stress responses. Scientific reports, 12(1), 19270. https://doi.org/10.1038/s41598-022-23222-9
24. Roussin, L., Gry, E., Macaron, M., Ribes, S., Monnoye, M., Douard, V., Naudon, L., & Rabot, S. (2024). Microbiota influence on behavior: Integrative analysis of serotonin metabolism and behavioral profile in germ-free mice. FASEB journal : official publication of the Federation of American Societies for Experimental Biology, 38(11), e23648. https://doi.org/10.1096/fj.202400334R
25. Ryu, S. W., Kim, J. S., Oh, B. S., Choi, W. J., Yu, S. Y., Bak, J. E., Park, S. H., Kang, S. W., Lee, J., Jung, W. Y., Lee, J. S., & Lee, J. H. (2022). Gut Microbiota Eubacterium callanderi Exerts Anti-Colorectal Cancer Activity. Microbiology spectrum, 10(6), e0253122. https://doi.org/10.1128/ spectrum.02531-22
26. Staudacher, H. M., Black, C. J., Teasdale, S. B., Mikocka-Walus, A., & Keefer, L. (2023). Irritable bowel syndrome and mental health comorbidityapproach to multidisciplinary management. Nature reviews. Gastroenterology & hepatology, 20(9), 582–596. https://doi.org/10.1038/s41575-023-00794-z
27. Stevens, B. R., Goel, R., Seungbum, K., Richards, E. M., Holbert, R. C., Pepine, C. J., & Raizada, M. K. (2018). Increased human intestinal barrier permeability plasma biomarkers zonulin and FABP2 correlated with plasma LPS and altered gut microbiome in anxiety or depression. Gut, 67(8), 1555–1557. https://doi.org/10.1136/gutjnl-2017-314759
28. Terlizzi, E. P., & Zablotsky, B. (2024). Symptoms of Anxiety and Depression Among Adults: United States, 2019 and 2022. National health statistics reports, (213), CS353885. https://pubmed.ncbi.nlm.nih.gov/39591466/
29. U.S. National Library of Medicine. (2024). Anxiety. MedlinePlus. https:// medlineplus.gov/anxiety.html
van
O’Sullivan, O., Clarke, G., Stanton, C., Dinan, T. G., & Cryan, J. F.
Short-chain fatty acids: microbial metabolites that alleviate stress-induced brain-gut axis alterations. The Journal of physiology, 596(20), 4923–4944. https://doi.org/10.1113/JP276431

Student Summer Research Projects
Research Models for Investigating Brain Tumors
by Tyler Truex
Reading Hospital Summer Student Intern, Department of Surgery
Preceptors:
Thomas Geng, DO, and Kathleen Lamb, MD
INTRODUCTION FOR BRAIN TUMOR MODELING TYPES
Innovations within brain tumor therapy have progressed slowly throughout the past several decades. Since the 1980s, the median survival period of patients exhibiting glioblastoma (GBM) has only improved by 3.7 months [5]. This lack of improvement is concerning, though it is not surprising, as Glioblastoma, or grade IV astrocytoma, is considered the most aggressive of primary brain tumor types [6]. This resistance to treatment stems from the vast heterogeneity of neoplasms found within the central nervous system (CNS).
Effective models should meet a set of key criteria: (1) replicate the same genetic variabilities, anatomical location, histopathological features, and development time frame as the parent tumor; (2) recapitulate intra- and intertumoral heterogeneity; and (3) reliably predict patients’ response to treatment.
GENETICALLY ENGINEERED MOUSE MODELS (GEMM)
Widely known as one of the most reliable mouse models, the genetically engineered mouse model utilizes knockout genes such as Cre-lox and Tet-inducible expression. Through the analysis of human tumors, tumor-driving mutations (e.g., EGFR, p53, PTEN) are delivered directly into the murine genome. This facilitates de novo tumor formation, mimicking the initial stages of glioblastoma genesis within an immunocompetent, vascularized host. Wide uses of GEMMs are found within the study of glioblastoma formation and to evaluate treatment responses within genetically determined contexts [6,7].
PROS OF THE MODEL
GEMMs replicate human biology and histology, while also maintaining an intact blood-brain barrier and tumor microenvironment. By avoiding injections, GEMMs avoid harming the blood brain barrier while maintaining integrity of the immune system. These models allow for specified manipulation of signaling pathways such as EGFR and PDGFR [6,7]. Notably, GEMMs have been beneficial for evaluating therapies such as
temozolomide (TMZ) and PARP inhibitor ABT-888, helping to clarify mutation-driven drug resistance and outcomes. For example, PTEN-mutant GEMMs exhibited increased sensitivity to merged TMZ and PARP inhibitor ABT-888 therapy compared to p53-mutants; GEMMs also allow evaluation of treatment outcomes in a vascularized, immunocompetent host [11].
CONS OF THE MODEL
GEMMs can form unwanted tumors in non-brain tissues due to the deletion of the tumor suppressor genes (e.g. p53), adding further complications to glioblastoma studies (e.g. CDKn2a-deficient mice develop lymphomas) [9]. GEMMs also require rigorous breeding plans with slow development and high cost [1,10]. Their tumors also frequently display lower genetic heterogeneity than human glioblastoma. Different mouse strain genetics and biological differences (e.g. telomere length) impact tumor characteristics and reduce direct human extrapolation [8]. While GEMMs sufficiently model specified mutations, they do not fully recapitulate the complexity of human tumor genetics.
RECENT FINDINGS
Recent studies using GEMMs have defined the role tumor suppressor pathways (e.g. Rb, Ras) play in glioblastoma development. In one study, inactivating the Rb pathway within mature fibrillary astrocytes via GFAP promoter-driven expression of a shortened SV40 T antigen led to 100% incidence occurrence at 300 days [12]. GEMMs expressing heterozygous PTEN deletion exhibited reduced disease-free dormancy while also developing higher grade tumors with increased cellularity and mitotic activity, marking PTENs role in glioblastoma progression and treatment resistance [12].
PATIENT DERIVED ORGANOIDS
PDOs are multicellular 3D cultures derived from patient tumor samples capable of maintaining the integrity of the original tumor’s physiology and function. They have become effective in vitro model systems to study cancer. Unlike 2D cultures, organoids are able to mimic the natural 3D microenvironment of a tumor.
The quality of an organoid depends on sample origin, culture technique used, and treatment history. Comprehensive glioblastoma PDOs retain driver gene expression and markers, such as Sox-2, Olig2, and EGFR [6]. Exemplary PDOs self-organize+, maintain genomic and phenotypic stability, self-renew, respond to stimuli, mimic tumor heterogeneity, and respond to drug treatments [2].
PROS
PDOs accurately mimic complex cell-to-cell interactions, such as malignancy and dormancy, while also modeling glioblastoma invasiveness; transplanted organoids migrate to brain satellite sites like tumors. Organoids provide promising platforms for personalized treatment development, exhibiting up to 81% sensitivity and 74% specificity in predicting patient response to therapy [2]. For example, PDOs derived from recurrent GBM patients with PTEN mutations and mTOR pathway activation were responsive to mTOR inhibitors, contributing to tumor decline [2]. PDOs also exposed mechanisms such as the role of the neuron-glioma synapse and involvement of NLGN3 in tumor growth; inhibition of NLGN3 suppressed tumor growth within organoid models [6].
CONS
PDOs require specialized labs, restricting availability for many communities. Furthermore, the process is often labor-intensive and time-consuming, requiring resources which many hospitals do not have. Distinct GBM subtypes, prominently IDH-mutant tumors, are harder to replicate than IDH-wildtype [4]. Some organoid procedures necessitate mechanical digestion of tumor tissue to conserve TME and the extracellular matrix. Organoids lack the vasculature and immune components needed for tumor biology and relapse [6]. Issues exist in enhancing subtype-specific culture protocols, expanding accessibility, and reproducing features such as the blood-brain barrier [6].
MODEL TYPE
ADVANTAGES
RECENT FINDINGS
PDOs have been utilized in modeling CAR-T cell therapy responses, exhibiting selective elimination of EGFR-expressing tumor cells and supporting EGFR as a dominant antigen in most patient cases [14]. PDOs also successfully mimicked patient tumor responses in vivo, highlighting their use in therapy outcome testing [13].
HEAD-TO-HEAD COMPARISON
Although each of the models retain key characteristics that make for better uses in different scenarios, several key statistics can be used to compare the two models head-to-head. First is the ability to accurately model patients’ tumor heterogeneity and outcomes of treatment. The PDO exhibits an average of an 84% success rate when modeling the original glioblastoma tumor heterogeneity [3,6]; this is high when compared to the modest average of 55% that the GEMM exhibits [8,10]. This high percentage exhibited by PDOs suggests their promising ability to be used in personalized treatments for glioblastoma drug testing.
Next, when analyzing the predictive accuracy for patient treatment outcomes, PDOs exhibit higher predictive power. As mentioned previously, in 2022, a study was conducted that determined PDOs exhibited 81% sensitivity and 74% specificity when predicting patient responses to therapies to GBM such as TMZ and mTOR [2]. Although GEMMs offer a live, vascularized host, to test therapies, their predictive power is lower at around 4060% depending on factors such as the mutation modeled and the TMZ [10,11,12].
Although these two metrics mentioned are key to glioblastoma modeling, an additional set of seven statistics demonstrate a strong correlation to the ability to accurately model glioblastoma.
DISADVANTAGES
Genetically Engineered Mouse Reliable, Tumor Growth De-Novo, Low-sample Throughput, Expensive, Model (GEMM) Blood-Brain Barrier Intact TME Different from Human [1,8,10]
Patient Derived Organoid
Short timeframe needed to Lack of normal brain tumor microenvironment, (PDO) establish PDOs and test lack of vasculature, and limited personalized therapies residual immune cells [6,16]
CHARACTERISTIC
Tumor Establishment Success
60-90% [3,4,6]
Time to Culture 2-6 weeks
Throughput
Invasion Modeling
Cost per model
High (100s)
90% show invasion
Medium
Ability to model subtypes Hard
Immune System/Vasculature
None
40-70%
3-6 months (Ready for Drug-Testing)
Low (>10)
Low percent of invasion (varying %)
High
Low with genetic alterations
Intact
Student Summer Research Projects
DISCUSSION/FUTURE DIRECTIONS
Both Genetically Engineered Mouse Models (GEMMs) and Patient-Derived Organoids (PDOs) provide key yet unique contributions to glioblastoma modeling. GEMMs provide the opportunity to study tumor formation and immune exchanges in vivo. On the other hand, PDOs provide a better model in preserving patient-specific tumor diversity and drug therapy development. Although overall advantageous, each offer a set of drawbacks as well—GEMMs being expensive and providing less genetic heterogeneity, and PDOs lacking vasculature and immune interactions; each still offers unique ways to tackle glioblastoma treatment. Work done to integrate these two models, such as mice with organoid grafts, should be made a primary focus to treat glioblastoma. By combining these two models, researchers can develop the most optimal glioblastoma treatment.

Tyler Truex is a junior at Eastern University, St. David’s, PA, majoring in biology with the intent to pursue a dual PhD-
4. Xu C, Yuan X, Hou P, Li Z, Wang C, Fang C. Development of glioblastoma organoids and their applications in personalized therapy. Cancer Biol Med. 2023;20(5):353–368. doi:10.20892/j.issn.2095-3941.2023.0061
5. Walid MS. Prognostic factors for long-term survival after glioblastoma. Perm J. 2008;12(4):45–48. doi:10.7812/TPP/08-027
6. Akter F, Simon B, de Boer NL, Redjal N, Wakimoto H, Shah K. Pre-clinical tumor models of primary brain tumors: Challenges and opportunities. Biochim Biophys Acta Rev Cancer. 2021;1875(1):188458. doi:10.1016/j. bbcan.2020.188458
7. Simeonova I, Huillard E. In vivo models of brain tumors: Roles of genetically engineered mouse models in understanding tumor biology and use in preclinical studies. Cell Mol Life Sci. 2014;71(20):4007–4026. doi:10.1007/s00018-0141675-3
8. Huszthy PC, Daphu I, Niclou SP, et al. In vivo models of primary brain tumors: Pitfalls and perspectives. Neuro Oncol. 2012;14(8):979–993. doi:10.1093/neuonc/nos135
9. Huse JT, Holland EC. Genetically engineered mouse models of brain cancer
888 therapy. Clin Cancer Res. 2014;20(10):2703–2713. doi:10.1158/1078-0432.CCR-14-
12. Hara T, Verma IM. Modeling gliomas using two recombinases. Cancer Res. glioblastoma complexity with organoids for personalized treatments. Trends Mol derived glioblastoma organoids as T cell therapy. Cell Stem
Racial Differences in Dietary Counseling Rates Among Patients with Post-Gastric Surgery Symptoms with History of Bariatric Procedure
by Austin Buskirk, John Fam, MD, Chief, Division of Bariatric Surgery, Thomas Geng, DO, Chief, Department of Surgery, Kathleen Lamb, MD, Vice Chair, Department of Surgery, Xuezhi (Daniel) Jiang, MD, Ph.D, Department of Obstetrics and Gynecology
Reading Hospital/Tower Health
Bariatric surgeries (BS) are procedures that are utilized to help assist patients with complicated obesity to achieve weight loss. The efficacy of these treatments is well documented; however, it is worth noting that a common side effect of bariatric procedures is dumping syndrome (DS), with as many as 10% of bariatric patients experiencing clinically significant DS symptoms. The presentation of DS can vary, but most patients experience gastrointestinal and vasomotor symptoms. While various treatment options exist for DS, the first-line treatment remains dietary counseling. To determine the rates of dietary counseling among DS patients of different races, we retrospectively studied the rates of dietary counseling of patients diagnosed with DS after BS utilizing the TriNetX Network.
We analyzed dietary counseling rates with race as an independent variable by conducting a chi-square test of independence (X 2 = 101.07, v = .109, p value = 3.14 x 10-20) as well as a residual analysis. We found that DS patients in the white racial category were statistically more likely to receive dietary counseling (sr = + 3.10). We also found that DS patients from the Other/Unknown, Black or African American, Native Hawaiian/Pacific Islander, and Asian racial categories were statistically less likely to receive dietary counseling (sr = -4.43, -2.02, -2.02. -2.02). DS patients from the Other/Unknown racial categories were least likely to receive dietary counseling. Similarly, when insurance and socioeconomic factors were accounted for, the dietary counseling rates with race as a variable again yielded statistical significance (X 2 = 35.01, v = .166, p value = .00000150).
We conclude that race has an impact on the likelihood that a

Student Summer Research Projects
Stroke Metrics and Functional Outcomes in Predominantly Spanish-Speaking Patients
by Arshia Chhabria, Ty Jozefick, Ricardo Ortiz-Loubriel, MD, Adam Sigal, MD, Traci Deaner, MSN, RN Department of Emergency Medicine, Reading Hospital/Tower Health
INTRODUCTION: Spanish is the second most spoken language in the United States, yet Spanish-speaking patients often face disparities in healthcare delivery and outcomes. Additionally, current data on the impact of limited English proficiency (LEP) on stroke care is often contradictory or contains several limitations. Anderson et al. found no differences in quality benchmarks and outcomes between predominantly English-speaking patients and Spanish-speaking patients (Anderson N., 2020). However, Vargas et al. noted worse neurologic outcome but no difference in functional outcome of Spanish-speaking patients in Texas (Vargas A., 2023). This study focused on investigating the effect of language disparity on quality benchmarks and outcomes in acute ischemic strokes (AIS).
METHODS: All patients with AIS, who were either Spanish or English speaking, presenting to Reading Hospital between January 2017 and December 2022 were included in the study. However, patients with spontaneous hemorrhagic strokes, patients with AIS being transferred to Reading Hospital, patients with a traumatic intracerebral brain hemorrhage, and patients with a prior stroke were excluded from the study. This retrospective study collected data about Demographics, Variable Times, and Outcomes. Comparisons between insurance status, area deprivation index (ADI) score, mean wait times for necessary procedures or scans, and outcomes through a 90-day Modified Rankin Score (MRS) for Spanish-speaking and English-speaking patients were analyzed with chi square, t-test, and logistic regression calculations.
RESULTS: There were 702 English-speaking patients and 119 Spanish-speaking patients in the study. 23% of English-speaking patients recorded a modified ranking scale (MRS) value from 3-6, indicating a poor outcome post hospital. 36% of Spanish-speaking patients recorded an MRS value from 3-6, indicating Spanishspeaking patients were more likely to experience a poor outcome after 90 days from hospital care. The p value was 0.017542, indicating that the data is significant. Spanish-speaking patients were more likely to have private or public insurance. The p value was less than 0.001. The differences can be attributed to a disparity in access to care. A logistic regression was used to control for the confounding variable of insurance to analyze if insurance metrics of Spanish-speaking AIS patients is independent of outcome compared to English-speaking AIS patients. This analysis resulted in a p-value of 0.104 which indicates data that is not statistically
significant. However, Spanish-speakers still had 1.61 times higher odds of poor outcomes. This suggests that insurance may be a confounding factor, though language still shows a trend toward worse outcomes. Additionally, there was a significant delay in the door to CT time (p-value = 0.004). The door to CTA/CTP and door to thrombectomy times were not significant (p-value = 0.14) and (p-value = 0.4). Both national and state ADI scores were significantly higher for Spanish-speaking patients (p-value < 0.0001), indicating a correlation between quality of care and worse socioeconomic disparities.
CONCLUSION: In this study, we conclude that language disparities may result in a lower quality benchmark of care and outcomes for patients presenting with acute ischemic strokes. For benchmarks like CT imaging, geographic socioeconomic factors, and functional outcomes it was clear that there was a variance in care for Spanishspeaking and English-speaking patients. Insurance may be a confounding factor in the MRS score results; however, further data collection is needed to supplement results with greater accuracy and significance. This study can translate into a Language Access Initiative where more awareness is placed on Spanish-speaking patients through stroke education and physician training for treating Spanish-speaking patients during high-acuity events like AIS.

Arshia Chhabria is pursuing a Bachelor’s degree in Biology at Virginia Commonwealth University, with plans to attend medical school after graduating in 2028. She is committed to serving others through medicine and is actively involved in research and community outreach.
Ty Jozefick is currently pursuing a Bachelor’s degree in Biological Sciences at Drexel University, with plans to attend medical school following his graduation in 2028.
References: Anderson N, J. A. (2020). Language disparity is not a significant barrier for time-sensitive care of acute ischemic stroke. BMC Neurology, 20, 363-368. Vargas A, Z. G. (2023). Stroke Outcomes Among English- and Spanish-Speaking Mexican Americans. Neurology. Doi: 10.1212/ WNL.0000000000207275
MESH vs ABCD2: Evaluating the MESH Score as a Clinical Decision-Making Tool for Risk Stratification of Ischemic Stroke after TIA
by William Davis, Peter Aziz, MS, Maxwell Studley, Ryan Gage, Leah Morgan
Preceptors: Tracie S. Deaner, MSN, RN, Adam Sigal, MD
Department of Emergency Medicine, Reading Hospital/Tower Health
INTRODUCTION: Stroke is the 5th leading cause of death and disability in the United States.1 Of the estimated 795,000 strokes occurring annually, 87% are estimated to be caused by an ischemic event, and 10-15% are preceded by a Transient Ischemic Attack (TIA).1,2,3 With nearly half of subsequent strokes occurring within 48 hours, rapid and accurate risk stratification in the emergency department is crucial.4 To meet this clinical need, the ABCD² (age, blood pressure, clinical features, duration of TIA, and presence of diabetes mellitus) score is a widely used tool, though its performance varies, with many studies citing a low specificity.3 A newer MESH score (antiplatelet/anticoagulant history, right bundle branch block, intracranial stenosis >50%, and hypodense area on CT ≥4cm), developed in an Asian population, has shown promising results but requires broader evaluation.
METHODS:
patients diagnosed with a TIA in the Reading Hospital emergency department. Data was collected to calculate the ABCD² score for each patient, and medical records were reviewed to identify subsequent ischemic strokes. The ABCD² score’s performance was evaluated based on its sensitivity, specificity, and the Area Under the receiver operating characteristic Curve (AUC).
RESULTS:
score demonstrated a sensitivity of 83.3% and a specificity of 20.6%. The AUC for the ABCD² score was 0.65, indicating fair discrimination. For comparison, the original MESH validation study reported a lower sensitivity of 71.4% but a dramatically higher specificity of 80.3% and an AUC of 0.81 for the MESH score in their population.
CONCLUSION:
functioned with high sensitivity but poor specificity, limiting its clinical utility. The fair discriminative performance of the ABCD²
score in this initial group underscores the need for a better risk stratification tool. While the MESH score’s lower sensitivity is a cause of concern, its superior specificity may make it a more practical tool for identifying patients who truly require admission and intensive workup. Completing our data collection will allow for a definitive evaluation and comparison of both the ABCD² and MESH scores’ predictive abilities at 2, 7, and 90 days post-TIA.
William Davis, whose hometown is Oley, PA, is a member of the Class of 2028 at Lake Erie College of Osteopathic


Student Summer Research Projects
Menopausal Hormone Therapy and Risk of Eczema in Postmenopausal Women: A Case-Control Study
by Anabelle Vue, Melodi Fugate, Leila Hashemi, DO, Xuezhi Jiang, MD, PhD Dept. of Obstetrics and Gynecology, Reading Hospital/Tower Health
OBJECTIVES: Eczema is a chronic inflammatory skin disease that disproportionately affects women and may be influenced by hormonal changes across the lifespan. Emerging evidence suggests that estrogen may modulate immune responses and skin barrier function, yet the association between Menopausal Hormone Therapy (MHT) and the risk of developing eczema later in life remains unclear. This study was conducted to investigate whether MHT use is associated with a reduced risk of developing eczema in postmenopausal women.
METHODS: We conducted an age-matched case-control study using retrospective data from a single institution between June 1, 2014, and May 31, 2025. A total of 155 women aged 45–70
RESULTS: There were no significant differences between cases and controls in mean age (60.8 ± 9.2 vs. 59.9 ± 9.5 years, respectively) or age at menopause (49.1 ± 5.2 years in both groups). Variables with a p-value <0.1 on univariate analysis, including BMI, ethnicity, alcohol use, and prior use of systemic MHT, were included in the multivariable logistic regression model. Hispanic/Latino ethnicity was significantly associated with a reduced risk of developing eczema (OR = 0.22, 95% CI: 0.056–0.89, p = 0.034), as was prior use of systemic MHT (OR = 0.21, 95% CI: 0.056–0.76, p = 0.018).
CONCLUSION: In this age-matched case-control study, systemic menopausal hormone therapy (MHT) and Hispanic/Latino

Melodi Fugate is an aspiring physician currently pursuing
Anabelle Vue is in her senior year at Millersville University
Berks County Medical Society Historical Center Dedicated in the Reading Hospital
by Eve Kimball, MD (BCMS Historian)
Michael Baxter, MD (Editor, the Medical Record)




One can imagine that an organization over 200 years old has quite a collection of artifacts and documents. That is certainly true for the Berks County Medical Society (BCMS) which recently dedicated our new Historical Center in the David George, MD, Library of the Reading Hospital. With the support of Charles Barbera, MD, President and CEO of Reading Hospital and a Past-President of the BCMS, and the tremendous efforts of Alexandra Short, MSLS, AHIP, System Director, Library Services, Tower Health, and Eve Kimball, MD, our BCMS Historian, a grand collection of portraits, books, documents, plaques and instruments (some nearly 200 years old) has been assembled. Central to the exhibit are the portraits of Isaac Hiester, the first President of the BCMS 1824-49, of Mrs. Paul C. Craig, President of the BCMS Women’s Auxiliary in 1935, of the Auxiliary of the PA Medical Society in 1948, and of the American Medical Association in 1957, and portraits of R. William Alexander, President of the BCMS in 1964 and the PA Medical Society in 1986, and Fay Weaver, MD, the first woman President of the BCMS in 1989.

There is a collection of fascinating books including early editions of Gray’s Anatomy texts and first editions of Frank Netter’s celebrated Atlas of Human Anatomy as well as many other texts and documents. There are copies of our BCMS publication, the Medical Record (originally the Medical Proceedings, founded in 1898) from the 1930s. Displays include several historical relics e.g. monaural stethoscopes, an obstetrical stethoscope, an early hemocytometer and scarificators used for “bloodletting.” Several documents and plaques commemorate past anniversaries and events including one very special one which celebrates the immense effort of our Medical Society physicians to immunize Berks County residents against polio for ten cents per dose with the Sabin vaccine in the early 1960s, a reminder that the BCMS has been dedicated to improving community health for 200 years (the focus was smallpox in 1824). There are several wood carvings by John Levan, MD, a former surgeon and master wood carver, and busts commemorating historical “pillars” of medicine: Imhotep, African/Egyptian Physician (2650-2575 BCE); Hippocrates, the great Greek physician (460-370 BCE); Moses ben Maimon known as Maimonides, the influential Spanish Sephardic Rabbi physician (1138-1204) and Canadian William Osler, MD, considered the “father of modern medicine” (1849-1919) who had a local Philadelphia connection through several institutions.
We invite all our members and anyone else who is interested in the history of medicine in Berks County to visit the new Historical Center in the Library on the third floor of the “B Building” Reading Hospital, hours 8:00 AM to 4:30 PM, Monday thru Friday. In our 201st year, we continue to celebrate our long tradition of promoting science-based patient care, education, collegiality and the highest standards of the medical profession.


COMMUNITY ANCHORS: HELPING HARVEST FRESH FOOD BANK
Challenging times have arrived for some of the community’s most vulnerable populations, including the Berks and Schuylkill County neighbors served by Helping Harvest Fresh Food Bank. These counties are home to over 72,000 adults and children living below the poverty line, plus more who live above the poverty line, but are food insecure.

What Helping Harvest Is and Who It Serves
Based in Reading, Pa., Helping Harvest is a Partner Food Bank of Feeding America, a nonprofit network of 199 food banks leading the fight against hunger in the United States.
Helping Harvest’s mission is simple: Feeding the hungry in Berks and Schuylkill counties. They gather food donations from grocery stores, farms, food manufacturers, food drives and individual donors, and sometimes purchase food. Food is sorted and stored in their warehouse, then distributed to neighbors through agency partners, such as food pantries, homeless shelters and meal programs as well as a few direct service programs.
The goal is to get nutritious food to the neighbors who need it most. Many people wrongly think they have a good idea what the typical food bank client looks like, yet there is no “typical” client among the neighbors Helping Harvest serves.
History and Evolution
Helping Harvest has been serving the community for over 40 years. Founded as the Greater Berks Food Bank (GBFB) in 1983, they distributed over 1 million pounds of food per year by their second year of operation. Five years after the organization’s founding, they became the Feeding America food bank for Schuylkill County as well.
In the 1990s, Helping Harvest expanded to include 45 agency partners and built a new facility in Muhlenberg Township. The next two decades saw continued growth including the launch of several programs like the Weekender Program, Healthy Sprouts and Mobile Markets, as well as a move to a larger facility, their current warehouse in Spring Township.
In 2019, GBFB rebranded as Helping Harvest Fresh Food Bank to better represent the organization’s commitment to providing nutritious food to both Berks and Schuylkill counties.
In 2020, during the COVID-19 pandemic, Helping Harvest distributed a record 11 million pounds of food. Since then, Helping Harvest acquired its first tractor-trailer; launched School Pantry and Maternal Health Programs and opened its second location, the Helping Harvest Community Kitchen.
In 2024, Helping Harvest distributed over 10.5 million pounds of food valued at almost $20.7 million.
Programs & Services
Helping Harvest has several ways they serve neighbors in coordination with approximately 350 agency partners, as well as direct service programs executed by their own staff and volunteers.

The food bank invests heavily in programs to support kids during their peak brain development years. The Weekender Program provides over 4,200 students weekly with bags of easy-toprepare meals and snacks to eat over the weekend. Healthy Sprouts provides bags of fresh foods to children in need in the City of Reading, with more than 1 million pounds of food distributed since its inception in 2010. The School Pantry Program gives middle and high school students plus their families access to food in a familiar environment. Finally, Helping Harvest is nearing the end of a two-year pilot of their Maternal

Health Program, funded by a Jewish Healthcare Foundation Healthy Food Access grant. This program provides boxes of nutrientdense foods to pregnant and postpartum individuals through partnerships with organizations such as WIC offices and Nurse Family Partnership programs.
Helping Harvest also supports senior citizens through their PA Senior Food Box Program which provides monthly food boxes to more than 2,100 low-income seniors. They also deliver fresh and frozen perishable foods to low-income senior housing facilities.
One of their most visible programs is the Mobile Market program with 24 Mobile Markets that provide a variety of nutritious produce, dairy and meat items along with shelf-stable products once a month at many locations.
The newest and most ambitious endeavor is the Helping Harvest Community Kitchen, opened in April 2025 adjacent to the Goggleworks Center for the Arts in downtown Reading. The Community Kitchen rescues bulk food from a variety of sources and produces heat-and-eat ready meals and repackages bulk food ingredients into family-friendly portions. To date, the Kitchen has produced over 20,000 heat-and-eat ready meals and repackaged over 7,000 units of rescued bulk food ingredients. In September 2025, Helping Harvest launched a hands-on culinary training program at the Community Kitchen in partnership with Reading Area Community College (RACC).
Helping Harvest provides additional supports with staff members, including a bilingual SNAP & Outreach Coordinator, available to connect neighbors with helpful services.
How You Can Help
Over a five-year span, the total value of food distributed by Helping Harvest more than doubled, jumping from $8.7 million in 2019 to $20.5 million in 2024. Federal funding cuts to programs like The Emergency Food Assistance Program (TEFAP), the Local Food Purchase Assistance Program (LFPA), SNAP and Medicaid, are severely compromising the effectiveness of nutrition programs aimed at increasing food security. Helping Harvest estimates that they will have 15% less food available, which equates to $3 million worth of
federally supported food per year that will no longer reach the local community.
As federal support continues to diminish, Helping Harvest will be more reliant on private fundraising and community support. There are several ways to help:
• Donate Food: Food donations helped make it possible for Helping Harvest to distribute almost $20.7 million worth of food last year. Learn more: helpingharvest.org/donate-food
• Donate Money: Relationships with retailers and the ability to bulk buy, allow Helping Harvest to purchase items at a fraction of the price. Learn more: helpingharvest.org/donate
• Donate Time: Volunteers sort and repack food donations, distribute food at Mobile Markets, prep food in the Kitchen and much more. Learn more: helpingharvest.org/volunteer
• Be an Advocate: Reach out to elected officials to ask them to restore vital programs and funding. Learn more: helpingharvest. org/advocate
• Spread the Word: Follow Helping Harvest on social media, sign up for E- News (by emailing marketing@helpingharvest.org), and spread the word to friends, family, colleagues and neighbors about Helping Harvest.

• Share Resources: Information about food assistance or SNAP application assistance can be found on Helping Harvest’s food map (helpingharvest.org/food-map) or directly at 610-926-5802 x206.
Helping Harvest remains committed to providing nutritious food for neighbors in need in Berks and Schuylkill counties, through tried-and-true methods, innovative initiatives and with a little help from their friends.

To learn more about the impact of Helping Harvest, visit HelpingHarvest.org and the food bank’s social media accounts, or reach out directly by emailing marketing@ helpingharvest.org.

Advances in Urology: Newer Diagnostic & Treatment Options for Prostate Disease
by Daniel Edwards, DO, FACS
Jacob Lucas, DO
Center for Urologic Care of Berks County
Nearly 2500 years ago Greek physician philosopher Hippocrates proclaimed, “I will not cut, even for the stone, but I will leave such procedures to the practitioners of that craft,” implying that these practitioners, primordial urologic surgeons, were uniquely well suited to the art of removing bladder stones.1 When we consider the process, which involved placing the patient in supine position with their legs elevated (hence ‘lithotomy positioning’), passing a curved metal rod per urethra to locate the stone by the sound it made as the rod tapped upon it (hence the medical instrument ‘urethral sound’ of the same name), then cutting through the perineum, sans anesthesia, until the neck of the bladder was entered and the stone could be removed, I suspect Hippocrates had good reason to ‘leave it to the professionals.’2
Given the ubiquity of urologic conditions, the impetus to innovate and evolve over time has been powerful among the urological community, and year after year we continue to see ongoing development of novel technologies, techniques and testing. For the medical community at large the awareness of these developments is important both for clinical context as they encounter patients who may have already undergone or are considering these therapies and the understanding to guide general questions regarding their indications.
For the purposes of this article, we will provide an overview of some of the most exciting, innovative and disruptive clinical developments to occur in urology in the past decade. We will highlight diagnostics and therapeutics in the management of some of the most common urologic entities: benign prostate hyperplasia, and prostate cancer detection and treatment
Benign Prostate Hyperplasia, or BPH, is one of the most common urologic conditions, which initially may present as early as age 40 and reach prevalence upwards of 60% by age 60 and 80% by age 80.3 The pathophysiology
involves obstruction of the prostatic urethral lumen by adenomatous prostate tissue.3 BPH alone is not a problematic condition, but contributes to declines in quality of life and places patients at risk of bladder dysfunction, incontinence, urinary retention, bladder stones, urinary tract infections and obstructive renal dysfunction and failure.4
For many decades, the gold standard endoscopic therapy for BPH has been transurethral resection of the prostate, or TURP, which involves endoscopic resection of prostate tissue transurethrally and, although very effective, has long term retreatment rates upwards of 7-15% and is associated with known side effects of retrograde ejaculation, and may also be associated with incontinence, limited changes in erectile function, and significant urinary bleeding.5,6 Transurethral laser photovaporization of the prostate was developed to limit bleeding, but many of the same other side effects remained.7 Transurethral laser enucleation of the prostate resulted in even more superior homeostasis and decreased retreatment rates, but did not solve the sexual dysfunction or incontinence conundrums.8
Two disruptive therapeutic approaches have been developed to drastically change the treatment landscape of BPH: mechanical retraction and transurethral ultrasound-guided waterjet ablation.
There are two guideline-directed procedural interventions which have used mechanical retraction to achieve the goal of increasing the lumen of the obstructed prostate: permanent prostatic urethral lift or PUL (UroliftTM) and temporary implanted prostatic devices or TIPD (iTindTM).
PUL utilizes a permanent suture implant deployed transurethrally through the prostate depositing a capsular tab that secures the implant to the “external” prostate wall, which is then tightened to retract the internal luminal
wall toward the capsule, then securing it in place with a small steel endpiece.9 Long-term efficacy suggests a 14% retreatment rate, comparable to TURP.9,10 Importantly, PUL has the lowest reported complication rate of all BPH interventions, lowest catheterization rate, and no effect on erectile or ejaculatory function or incontinence.11,12
TIPD utilizes a pyramid-shaped stent that is deployed via cystoscope that manually retracts the obstructive lobes of the prostate.13 It is left in place for 5 to 7 days and then retrieved via a urethral tether and specialized catheter. It offers modest improvements in urinary flow and quality of life with no impact on sexual function, but currently long-term data is lacking.14,15
For patients who are not optimal candidates or fail these less-invasive treatment options, Robotic waterjet treatment (RWT) is an attractive alternative with excellent outcomes. RWT utilizes an endoscopic robotic arm as well as a transrectal ultrasound probe. A high-powered waterjet is used to ablate obstructive prostate tissue and treatment planning occurs using high-quality transrectal ultrasound and artificial intelligence programming.16 By identifying important structures on the transrectal ultrasound, such as the bladder neck, ejaculatory ducts and urethral sphincter complex, the treatment is able to avoid these structures and preserve ejaculatory and erectile function as well as continence.17 Additionally, by avoiding electrocautery or thermal energy throughout the majority of the procedure, scarring is minimized. Unlike the other procedures mentioned, RWT is size-independent, thereby allowing us to treat large glands endoscopically in minimal time, while again preserving those incredibly important bodily functions to a greater degree than other resection or ablationtype procedures.18,19
Unfortunately, another common urologic affliction remains prostate cancer (CaP). CaP
affects many men, with up to 1 out of 8 men being diagnosed with prostate cancer over the course of a lifetime.20 CaP is the leading non-skin cancer diagnosis among men and the second leading cause of cancer death.20,21 Prostate-specific antigen (PSA) screening has been shown to reduce the risk of CaP mortality by 25-50% and the risk of metastatic disease by up to 40%, but results in many false positives, or diagnosis of clinically insignificant cancer, both of which can result in unnecessary treatment burden and psychologic distress.22-24 However, for patients who have elevated PSA readings or are at higher risk of cancer due to individual factors, urologists have gained two tools which significantly improve our detection rates of clinically significant cancer and decreased our false positive rates: MRI of the prostate gland as well as novel biomarkers.
MRI of the prostate is not a new technology, but its importance in adjudication of an elevated PSA has become increasingly standard of care over the past several years and cannot be understated. Large trials have demonstrated that utilizing MRI routinely as further adjudication of an elevated PSA results in over 50% greater detection of clinically significant cancer, and greater than 50% decreased detection of low-grade cancers likely to be clinically insignificant.25 For many patients, this may help them to avoid an unnecessary biopsy. For others, this may help them better identify a lethal cancer. However, MRI may carry upwards of a 15-20% false negative rate, and some patients may be unable to obtain MRI due to clinical contraindications. For these patients, PSA-independent testing is of the utmost importance. Fortunately, there are numerous urinary tests, both with and without simultaneous digital rectal exam, that are validated to identify expression of DNA biomarkers within the urine that are associated with the presence of clinically significant prostate cancer. Tests such as SelectDXTM, ExoDXTM and MPSTM (My Prostate Score) are able to avoid unnecessary biopsies by up to 35% in patients who, by PSA criteria alone, may have received a biopsy unnecessarily, while suffering a false negative rate of only 5-10%.26-30 A newer serum-based test, EpiSwitchTM, reports excellent specificity and sensitivity, although it has yet to be recommended in current guidelines. Tests such as these can help navigate the shared decision making that is so important in the screening and diagnosis of CaP.
For patients who have been diagnosed with prostate cancer, treatment options historically have included surgery to remove the prostate, or radiation to the prostate with or without burdensome hormone therapies. For patients with low to favorable intermediate risk prostate cancer, active surveillance (AS) has become a standard of care practice for many patients, although 50% of patients on AS will eventually convert to definitive therapy,
and active surveillance across all disease stratifications results in about double the risk of metastases.32 For some patients with low or intermediate risk disease, the prospect of radical therapies such as surgery or radiation and the associated risks and side effects may be overwhelming, or simply AS may not seem like treatment enough. For those patients, a promising alternative is the realm of focal and ablative therapies for prostate cancer, of which high-intensity focused ultrasound, or HIFU, has risen to the forefront. HIFU uses a transrectal ultrasound probe which is able to both provide imaging ultrasound as well as targeted high-intensity ultrasound that focuses the energy on a few millimeters of tissue at a time, heating the tissue and causing cancer cell death.33 With HIFU, a treating physician can target a small area such as may be identified on an MRI, or could treat a quadrant, hemi-gland or whole gland depending on the patient’s disease characteristics.34 Although longterm data is lacking, current studies suggest that 10% of patients may require a repeat treatment, but 70% of patients or more are able to avoid treatment failure or progressing to radical therapies up to seven years later.35 Furthermore, rates of erectile dysfunction and incontinence, some of the most worrisome side effects of traditional prostate cancer treatment, are reported at or below 5%, and up to 0% for patients with highly focal areas of treatment.36 While this treatment option requires optimal patient selection and not all patients will qualify for HIFU as an optimal therapy, it remains an important tool in our armamentarium.
The field of urology remains highly dynamic, and innovations in diagnostics and therapeutics abound across the specialty. Undoubtedly, decades of evolution have led to overall improvements in patient quality of life, decreases in disease morbidity and waning treatment-related burden. We have come a long way since implicated by Hippocrates all those millennia past, but certainly the future ahead remains promising.

1. All the Hippocratic passages are deriving from the translation of Hippocrates by Loeb Classical Library. I-VIII. Cambridge, MA: Harvard University Press; 1923. 1995.
2. John Herman. Urology: A View Through the Retrospectroscope. Harper & Row Publishers; 1973. The Hippocratic Oath. National Library of Medicine.
3. Berry SJ, Coffey DS, Walsh PC et al: The development of human benign prostatic hyperplasia with age. J Urol 1984; 132: 474.
4. O’Leary MP: Luts, ed, qol: Alphabet soup or real concerns to aging men? Urology 2000; 56: 7
5. Taylor BL and Jaffe WI: Electrosurgical transurethral resection of the prostate and transurethral incision of the prostate (monopolar techniques). Can J Urol 2015; 22 Suppl 1: 24
6. Lourenco T, Shaw M, Fraser C et al: The clinical effectiveness of transurethral incision of the prostate:
A systematic review of randomised controlled trials. World J Urol 2010; 28: 23.
7. Bouchier-Hayes DM, Van Appledorn S, Bugeja P et al: A randomized trial of photoselective vaporization of the prostate using the 80-w potassium-titanylphosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int 2010; 105: 964.
8. Elshal AM, Soltan M, El-Tabey NA et al: Randomised trial of bipolar resection vs holmium laser enucleation vs greenlight laser vapo-enucleation of the prostate for treatment of large benign prostate obstruction: 3-years outcomes. BJU Int 2020; 126: 731.
9. Roehrborn CG, Barkin J, Gange SN et al: Five year results of the prospective randomized controlled prostatic urethral l.I.F.T. Study. Can J Urol 2017; 24: 8802.
10. Gratzke C, Barber N, Speakman MJ et al: Prostatic urethral lift vs transurethral resection of the prostate: 2-year results of the bph6 prospective, multicentre, randomized study. BJU Int 2017; 119: 767
11. McVary KT, Gange SN, Shore ND et al: Treatment of luts secondary to bph while preserving sexual function: Randomized controlled study of prostatic urethral lift. J Sex Med 2014; 11: 27
12. Woo HH, Bolton DM, Laborde E et al: Preservation of sexual function with the prostatic urethral lift: A novel treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med 2012; 9: 568.
13. Chughtai B, Elterman D, Shore N, et al. The iTind Temporarily Implanted Nitinol Device for the Treatment of Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia: A Multicenter, Randomized, Controlled Trial. Urology. 2021.
14. De Nunzio C, Cantiello F, Fiori C, et al. Urinary and sexual function after treatment with temporary implantable nitinol device (iTind) in men with LUTS: 6-month interim results of the MT-06-study. World J Urol. 2021.
15. Elterman D, Alshak MN, Martinez Diaz S et al: An evaluation of sexual function in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia in men treated with the temporarily implanted nitinol device. J Endourol 2023; 37: 74.
16. Gilling PJ, Barber N, Bidair M et al: Randomized controlled trial of aquablation versus transurethral resection of the prostate in benign prostatic hyperplasia: One-year outcomes. Urology 2019; 125: 169.
17. Gilling P, Barber N, Bidair M et al: Three-year outcomes after aquablation therapy compared to turp: Results from a blinded randomized trial. Can J Urol 2020; 27: 10072
18. Gilling P, Barber N, Bidair M et al: Water: A double-blind, randomized, controlled trial of aquablation(®) vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol 2018; 199: 1252.
19. Plante M, Gilling P, Barber N et al: Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: Subgroup analysis from a blinded randomized trial. BJU Int 2019; 123: 651.
continued on next page >
Advances in Urology: Newer Diagnostic & Treatment Options for Prostate Disease
Berks County Medical Society Alliance Celebrating 100 Years of Service at the Doctor’s Grove
by Mansi Vasconcellos, MD President, The Berks County Medical Society Alliance
The Berks County Medical Society Alliance spent a beautiful morning at the Doctor’s Grove located near the Berks County Heritage Center. The Doctor’s Grove was founded in the 1980s as a tribute to the lives and work of beloved physicians in our community. The Grove has grown and now has approximately 80 trees dedicated to individual physicians. There are approximately three trees waiting to be planted. We are always appreciative of donations to this local community treasure. Visit this peaceful and scenic place with your family sometime soon and pay respect to our medical community!

Our Centennial philanthropy efforts are underway! We are collecting “100 books for 100 years” at our Fall events and we hope to reach that goal quickly—we already have 57! Books will be distributed to pediatrics practices seeing primarily Medicaid patients to promote childhood literacy. Our next event was the morning of October 7 when we toured the Reading Hospital to learn about the pediatrics and geriatrics services offered to the community.
Visit our website or social media pages to contact us for more information about our events. And please look out for an invitation to the Centennial Event we have planned in early November where we can meet, socialize, and celebrate a century of philanthropy. Fundraising from this event will be used to create a new need-based financial hardship fund for medical trainees. Stay tuned for more information and we hope to see you there!

continued from page 31
20. Siegel RL, Miller KD, Wagle NS et al: Cancer statistics, 2023. CA Cancer J Clin 2023; 73: 17
21. Rawla P: Epidemiology of prostate cancer. World J Oncol 2019; 10: 63
22. Hugosson J, Roobol MJ, Mansson M et al: A 16-yr follow-up of the european randomized study of screening for prostate cancer. Eur Urol 2019; 76: 43
23. Hugosson J, Godtman RA, Carlsson SV et al: Eighteen-year follow-up of the goteborg randomized populationbased prostate cancer screening trial: Effect of sociodemographic variables on participation, prostate cancer incidence and mortality. Scand J Urol 2018; 52: 27
24. Gronberg H, Adolfsson J, Aly M et al: Prostate cancer screening in men aged 5069 years (sthlm3): A prospective population-based diagnostic study. Lancet Oncol 2015; 16: 1667
25. Kasivisvanathan V, Rannikko AS, Borghi M et al: Mri-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 2018; 378: 1767
26. Eyrich NW, Morgan TM and Tosoian JJ: Biomarkers for detection of clinically significant prostate cancer: Contemporary clinical data and future directions. Transl Androl Urol 2021; 10: 3091
27. Hendriks RJ, van der Leest MMG, Israel B et al: Clinical use of the selectmdx urinary-biomarker test with or without mpmri in prostate cancer diagnosis: A prospective, multicenter study in biopsy-naive men. Prostate Cancer & Prostatic Diseases 2021; 3: 03
28. Lebastchi AH, Russell CM, Niknafs YS et al: Impact of the myprostatescore (mps) test on the clinical decision to undergo prostate biopsy: Results from a contemporary academic practice. Urology 2020; 145: 204
29. Lendinez-Cano G, Ojeda-Claro AV, Gomez-Gomez E et al: Prospective study of diagnostic accuracy in the detection of high-grade prostate cancer in biopsy-naive patients with clinical suspicion of prostate cancer who underwent the select mdx test. Prostate 2021; 81: 857
30. McKiernan J, Donovan MJ, Margolis E et al: A prospective adaptive utility trial to validate performance of a novel urine exosome gene expression assay to predict high-grade prostate cancer in patients with prostate-specific antigen 2-10ng/ml at initial biopsy. European Urology 2018; 74: 731
31. Dmitri Pchejetski, Ewan Hunter, Mehrnoush Dezfouli, Matthew Salter, Ryan Powell, Jayne Green, Tarun Naithani, Christina Koutsothanasi, Heba Alshaker, Jiten Jaipuria, Martin J. Connor, David Eldred-Evans, Francesca Fiorentino, Hashim Ahmed, Alexandre Akoulitchev, Mathias Winkler. Circulating Chromosome Conformation Signatures Significantly Enhance PSA Positive Predicting Value and Overall Accuracy for Prostate Cancer Detection. Cancers, 2023; 15 (3): 821
32. Hamdy FC, Donovan JL, Lane JA et al: 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Eng J Med 2016;375:1415
33. Hopstaken JS, Bomers JGR, Sedelaar MJ et al: An updated systematic review on focal therapy in localized prostate cancer: what has changed over the past 5 years? Eur Urol 2022; 81: 5
34. Bates AS, Ayers J, Kostakopoulos N et al: A systematic review of focal ablative therapy for clinically localised prostate cancer in comparison with standard management options: limitations of the available evidence and recommendations for clinical practice and further research Eur Urol Oncol 2021;4:405.
35. Shah TT, Reddy D, Peters M, Ball D, Kim NH, Gomez EG, Miah S, Evans DE, Guillaumier S, van Rossum PSN, Van Son MJ, Hosking-Jervis F, Dudderidge T, Hindley R, Emara A, McCracken S, Greene D, Nigam R, McCartan N, Valerio M, Minhas S, Afzal N, Lewi H, Ogden C, Persad R, Virdi J, Moore CM, Arya M, Emberton M, Ahmed HU, Winkler M. Focal therapy compared to radical prostatectomy for non-metastatic prostate cancer: a propensity score-matched study. Prostate Cancer Prostatic Dis. 2021 Jun;24(2):567-574.
36. Reddy D, Peters M, Shah TT, van Son M, Tanaka MB, Huber PM, Lomas D, Rakauskas A, Miah S, Eldred-Evans D, Guillaumier S, Hosking-Jervis F, Engle R, Dudderidge T, Hindley RG, Emara A, Nigam R, McCartan N, Valerio M, Afzal N, Lewi H, Orczyk C, Ogden C, Shergill I, Persad R, Virdi J, Moore CM, Arya M, Winkler M, Emberton M, Ahmed HU. Cancer Control Outcomes Following Focal Therapy Using High-intensity Focused Ultrasound in 1379 Men with Nonmetastatic Prostate Cancer: A Multi-institute 15-year Experience. Eur Urol. 2022 Apr;81(4):407-413.
2025 BCMS Night at the Reading Fightin’ Phils
Over 80 Berks County Medical Society members, residents, and Drexel University Medical Students registered to join our annual night at the ballpark on Thursday, August 14th, with a pool party, picnic buffet, ballgame, and fireworks.
BCMS President Ankit Shah, MD, threw out a first pitch strike (which appeared to be a nasty curve ball) with the support of his sidekick “Screwball” (see picture). The group enjoyed an evening of warm camaraderie (one of our key BCMS Compass Points) which concluded with a great fireworks display.
Everyone—kids, families, students, and the “old timers”—had a great time, a perfect August evening and a great introduction to the Reading/ Berks community for our Drexel students. This event continues a great partnership between the BCMS and the Reading Fightin’ Phils.
Our annual night at the Reading Fightin’ Phils is always a great event to meet new members and share some fun together.











Resident Rounds: When Algorithms Are Not Enough
by Fatima Khalid, MD, PGY 3, Reading Hospital Internal Medicine Residency
“Argh – I just got another patient added to my list; it’s an acute visit.”
“What is the acute visit for?”
“Increased anxiety?”
I talk to my co-resident as I sift through my schedule for the day.
“The patient has been roomed—she is hysterically crying and inconsolable,” I read from the secure chat as I quickly peruse her chart.
My heart skips a beat—despite doing this for more than a year now, seeing patients intubated and calling out the time of death, my heart still occasionally experiences a double take when I see or hear somebody crying. There is just something about the reality of a human being crumbling under the weight of their emotions.
I walk over to the room and see the patient folded in on herself on the floor, hugging one of the nurses with tears streaming down her face.
I squat on the floor and pat her shoulder—but she flinches, moving away from my touch. Cautious, I step back.
Tentatively, I ask: “How can I help you?”
“Make it stop, please make the voices in my head stop—I cannot breathe,” she desperately replies.
My heart constricts upon itself. I try to keep a poised face and reach for her hand again: “Talk to me—what is going on?”

As per her chart, she has been struggling with increased anxiety for about 20 years now—ever since she got out of an abusive marriage. Through a long struggle in court to gain custody of her children and then raising them alone in this economy, she has endured so much.
This was my first time seeing her. In broken sentences, she began to narrate how everything has been so hard recently: how she has not been on good terms with her children, how she has not seen her grandchildren in about five months, how her daughter is struggling with drug addiction and is reportedly homeless now, how another son is struggling with bipolar disorder and his manic episodes remind her of their father and trigger her. How she recently lost her job, has been unable to take her medications—and how everything has just been difficult to manage.
As I listen and slowly pat her shoulder, something begins to crumble inside me. My brain, used to the algorithms of management, begins to swiftly work through them, trying to find which one to follow.
She squeezes my hand as her crying comes to a standstill. With empty, misty eyes she tells me she has been going to therapy weekly, mentions the medications she has been on in the past, and asks for some refills so she can hopefully get better.
I talk through the scores and ask about her symptom—to classify her, group her, put her in a category—so I can
decide the medication regimen. But even as I do so, a tiny, mad-at-the-world voice tells me: “You can’t fix this. You can’t fix somebody’s life and the unfairness of it with an SSRI.”
I did what I got my degree for—I provided her with refills on medications, told her to follow up with her therapist, and scheduled a six-week follow up.
As I walked out of the room, on days like this, I get humbled by life.
Who knows how she will manage in six weeks? Will the racing thoughts stop? Will she be able to meet her grandchildren? Will her daughter find housing? Will her son be better? Will she be able to find a job?
Mental health is real—and it is important, the awareness, the medications, the help. It helps a lot of people. But it is not lost on me as I see my patients, that some of it—sadly, more than I want—is secondary to unfair life. It is due to factors I cannot control, and all I can do is try my best to give them the tools to deal with it better. But it humbles and hurts me that some days; I just cannot fix people.
Painful as it may be, I think realizations like this are important, because they remind us of something which is not part of our management algorithms—empathy. Holding someone’s hand, passing them a box of tissues, spending those extra 15 minutes with them in silence. A silent vow of solidarity. It may or may not help—but on days like this, I am willing to try everything.

School Absenteeism and How Physicians Can Help
by Betsy Adams, Ed.D Coordinator of the Berks Initiative for School Attendance
Do you know that of students who missed 18 or more days of school in 6th grade, 75% will go on to drop out of high school? If a student misses 18 or more days in kindergarten and again in 1st grade, only 17% will be able to read on grade level in 3rd grade? Those are some of the alarming statistics that show the impact of chronic absenteeism. Chronic absenteeism is defined as missing 10% or more of the school days, or 18 days in a year, FOR ANY REASON. Before 2018, 15% of students across the United States were chronically absent. This increased to 30% during the pandemic and has been reduced only slightly since then. In 2324, 22% of students were chronically absent.
Why Should Health Professionals Care?
Leaders in public health and education see chronic absence as a public health challenge. “Attending school regularly is one of the most powerful predictors of long-term health, well-being and success,” said Josh Sharfstein, MD, Director, Bloomberg School of Public Health. Chronic absence “is a signal like a vital sign that something in the child’s world isn’t working as it should.” Chronic absenteeism is associated with engaging in health risk behaviors, including smoking cigarettes or marijuana, alcohol and other drug use, and risky sexual behavior. Poor school attendance is also associated with juvenile delinquency; 78% of students arrested have been chronically absent before the arrest.
What can a Physician Do About It?
The American Academy of Pediatrics Policy Statement of February 2019 says: “Routinely ask at preventive care visits and sick visits about the number of absences a student has experienced.” Ask about the number of days missed in the past month but know that parents routinely underestimate this number. Consider asking the child or parent to pull up student information on the school’s portal so the physician can see grades and attendance. Stress the value of developing strong school attendance habits as early as preschool.
When is Sick Too Sick for School?
Help the parents understand when a student can go to school and when they need to stay home. From the AAP policy statement: “Avoid writing excuses for school absences when the absence was not appropriate. Encourage patients who are well enough to return to school immediately after their medical appointments.” Get a school calendar and daily schedule so that the office can schedule appointments on days when there is no school or before or after the school day.
Build the School Physician Partnership
All schools in Pennsylvania have a school nurse, the best medical partner for the physician. School nurses can help with individual student plans for chronic illnesses such as asthma, migraines, diabetes, etc. The school can provide contact information for the school nurse and social worker for each building.
Schools have information that a physician can use to help a client. The counseling office or school social worker can provide information about
resources available for food, transportation, housing, etc. Physicians can refer a student or family to the Student Assistance Team who will collect information from people who know the student and determine if additional help is needed such as counseling, mental health assistance, drug/alcohol, etc. Physicians can help by answering questions from the school nurse who may contact them when a student has many absences or a serious medical condition. The nurse can discuss what can be done at school to accommodate the student in school instead of being absent. The nurse might discuss the number of absences and the impact on the student. Sometimes physicians are asked by a parent to provide a note requesting an evaluation for a 504 plan or IEP to address health barriers. However, the parent must first sign the school’s legal documents before the evaluation can begin.
What About School Anxiety?
The start of a new school year stirs up anxiety. So does a test, or worries about clothes, hair, friends, etc. School-related anxiety is estimated to represent anywhere from 5 to 12% of pediatric office visits which may manifest as an upset stomach or a headache.
The counseling office, school social worker, administrator, or others can assist the student who has school anxiety. Depending on the severity of the problem, schools can provide counseling, change schedules, provide emotional support or even a special school.
Berks County Information
The chronic absence rate in Berks County is better than the national average, but individual schools have chronic absence rates ranging from only 5% chronically absent to 55% of students chronically absent. Schools regularly review attendance data to see which students are missing more than 10% of the days. The school will take steps to understand why the student is missing and see how to get the student to attend more regularly. Discussions will be held with the student and parent, possibly holding a Student Attendance Improvement Conference (SAIC) and writing a Student Attendance Improvement Plan (SAIP) which are required before any legal steps can be taken. Those meetings could include physicians if appropriate. Schools can also refer students and families in Berks County to the Advancing School Attendance Program (ASAP), part of SAM, which provides case management help to families to improve attendance. This program is free to schools and families and if parents cooperate, over 95% of the students improve their attendance. Physicians can also refer students.
Conclusion: If physicians and schools work together, we can have more students attending regularly, getting better grades, leading healthier lifestyles, and having a more healthy, productive life.

Other contributors to this article include: Anne Fisher, M. Ed., BSN, Director of Student Support Services, Reading School District; Olubunmi Ojikutu, MD, Chair of Pediatrics, Reading Hospital/Tower Health, and Mansi Vasconcellos, MD, Pediatric Hospitalist, Reading Hospital/Tower Health.
Student Vital Signs

As I sat down in the physicians’ lounge to sift through all the details of my patients’ charts assigned to me for the day, I came across a patient with an extensive problem list. Paul had been on the inpatient unit for four days, but it was my first day on his care team. Up to that point, it was my fourth week out of my eight-week long internal medicine rotation. I jotted down the questions to ask my patients as I finished my chart review, highlighting the ones that pertained to possible acute overnight events. I sat up, quickly noted the floors and room numbers of my patients, and put on my overworn whitecoat, making sure the bell of my stethoscope was on my right (for whatever reason it felt better that way). I decided to go see Paul first and as I speed-walked to his room, I was hit by this breeze of cold air that seems to circulate throughout all hospital hallways. It carried me back to the days when I had wished to be exactly where I was in that moment— stepping into the real world, finally becoming part of the medical team, and playing a part, however small, in alleviating someone’s suffering. But Paul had already gone to dialysis by the time I made it to his room, so I decided to circle back to him later in the dialysis unit.
That One Patient
by Peter Aziz, MS lll, Drexel University College of Medicine
Paul was 59 years old. Over my weeklong interaction with him, I learned that he was married and that he was interested in fishing but never had the chance to go. He was also interested in different cultures and languages and liked learning about them. Looking back, I never got a chance to ask about his occupation or whether he had children, and he never brought up those topics either. Overall, he was an approachable individual, but his problem list was not. He suffered from multiple myeloma and end-stage renal disease. Chemotherapyinduced immunosuppression had allowed his varicella-zoster virus to reactivate, causing very painful shingles. Because his treatment required properly functioning kidneys, lower doses had to be administered; consequently, the infection spread to his brain.
The dialysis unit never fails to amaze me—a vast room with rows of machines and patient beds. Before medical school, I cared for many dialysis patients as part of my medical-transportation job. This patient population is unique in that it requires unparalleled grit and patience to be connected to a kidney-replacing machine while most of your blood is getting circulated through, a process that takes nearly three hours and occurs about two to
three times weekly. Patients who rely on this form of dialysis are usually very sick. Paul’s illness, however, was further complicated by his infection.
When I walked in, Paul was lying in his bed, and I could hear his blood bumping through the machine and back to his body. His wrists and ankles were secured to the bed. He had been shouting random words and seemed to be aggressive before I came in. He ultimately had to be placed in soft restraints. There was no point in introducing myself or asking about overnight events because Paul did not know where he was. He was disoriented. His mentation was altered, and his thought process and speech were incoherent and disorganized. None of it was his fault or intentional. Later that day, I called his wife to update her, and it was an unusual feeling to be the one updating a patient’s family member. I could hear the sadness in her voice as she learned that her husband was not his usual self. My attending physician had agreed prior to calling that his case is more of a watch-and-wait situation, adding more uncertainty to my update to Paul’s wife.
The next few days followed a similar pattern: rounding on Paul, updating his wife, and keeping an eye out for any acute

events. By my third day caring for him, he was a completely different person—fully alert and oriented to himself and surroundings. This stark contrast made me reflect on how the state of disease can wholly alter a person’s psyche. Illness can create versions of a person that are unknown, distorted, and deeply vulnerable. On that day, I learned about his interest in going fishing. His infection had caused painful blisters on his back, but overall, he was clinically stable—or so we thought.
Over the next two days, Paul’s condition deteriorated rapidly, in a way that no good clinical acumen could have predicted. Later I learned that he suffered a cardiac arrest, and a code blue was called. He was resuscitated, intubated, and transferred to the ICU. Shortly after, his wife made the difficult decision of placing him under a DNR/DNI status, and comfort measures were initiated.
As medical students, we are often told that we have more time to process the vast amount of information that accompanies the patients assigned to us; after all, patients serve as our greatest teachers during third year. But we must also process the emotions that come with caring for them. Paul’s case will have a lasting impact on my journey. His rapid decline, my daily updates to his wife, and our interactions will serve as a powerful reminder of why I chose this profession in the first place.


2025 Global Impact Conference & Annual FaithCare Banquet
CONFERENCE
October 24 • noon - October 25 • 3:30 pm 1025 Old Wyomissing Rd. • Reading, PA
BANQUET
October 25 • 5 pm Spring Valley Church 2727 Old Pricetown Rd. • Temple, PA
Share Health, Hope, and Healing with Us!
Join hundreds of healthcare professionals, students, and community members to be inspired, connect, and make a global impact. At the conference, hear powerful stories, engage in thought-provoking debate, and discover mission opportunities around the world.
Cap it off at the Banquet - a joyful evening with delicious food, live music, auctions, prizes, and the chance to encourage this life-changing ministry.
Sponsorships Available
email hope@faithcare.net for details
Scan the QR code to learn more, register, and donate. *

*Alternatively, donations may be mailed by check to FaithCare, 621 Centre Ave, Reading, PA 19601
*FaithCare is a Christiam Faith-based organization which provides medical care and spiritual support to those in need around the world. FaithCare has a monthly Free Clinic in Reading. For more information see contact information.


PAMED Advocacy in Action: Updates from D.C. and Harrisburg
As Pennsylvania nears the end of the 2025–2026 fiscal year, the state legislature remains mired in negotiations over the still-unpassed 2026 budget. The prolonged impasse, now entering its third month, has slowed legislative momentum in Harrisburg, leaving many bills in a holding pattern.
Despite the lull, PAMED continues to advocate on key issues— including its recent opposition to the federal “Equitable Community Access to Pharmacist Services Act” (ECAPS). Alongside the AMA and other physician groups, PAMED has raised serious scope-ofpractice concerns, warning that the bill’s expansion of pharmacists’ clinical authority could compromise patient safety and fragment care.
As budget talks continue, PAMED remains focused on monitoring several state-level bills that could resurface once negotiations conclude.
Bill for Diagnostic Breast Exam Coverage Advances
The Pennsylvania House passed House Bill 433, which mandates health insurance coverage for all costs associated with diagnostic breast imaging. Introduced by Rep. Gina Curry (D–Delaware County), the bill defines diagnostic imaging to include diagnostic mammography, breast MRI (standard or abbreviated), and breast ultrasound. HB 433 seeks to expand current protection to follow-up imaging when abnormalities are found. The bill now awaits action in the Senate.
Cannabis Legalization Stalls in Senate
House Bill 1200, which proposes legalizing adult-use cannabis in Pennsylvania, narrowly passed the House with a 102–101 vote. The bill would allow adults age 21 and older to purchase cannabis through a regulated system and includes provisions for personal cultivation, expungement of certain low-level convictions, and reinvestment of tax revenue into community programs. After referral to the Senate Law and Justice Committee, the bill failed to advance following a vote on May 13.
PAMED continues to oppose broad-based use of cannabis as medicine, advocating instead for rigorous clinical research and trials. While PAMED supports the decriminalization of personal use, it does not endorse full legalization. If legalization proceed, PAMED insists it must be accompanied by a robust regulatory framework—
such as the one outlined in HB 1200—to mitigate harm and safeguard public health.
Oversight of Health Care Transactions Involving Private Equity
House Bill 1460, introduced by Rep. Lisa Borowski (D–Delaware), seeks to enhance oversight of major health care transactions involving private equity and large health systems. The bill requires advance approval from the Department of Health and the Attorney General, boosts transparency, and restricts saleleaseback arrangements.
PAMED supports HB 1460 in alignment with its commitment to transparency and accountability in health care operations. The bill was reported as amended and received its first consideration in the House on June 3. It has since been re-committed to the House Rules Committee for further review.
Supporting Primary Care in Underserved Areas
House Bill 425, introduced by Rep. Kristin Marcell (R–Bucks), proposes the creation of a grant program to support J-1 visa physicians practicing in underserved communities. Employers of physicians with a Conrad 30 waiver would be eligible to apply for funding to help offset salary costs.
PAMED endorses HB 425 as a strategic measure to improve access to primary care across Pennsylvania. The bill was reported as amended and received its first consideration in the House on June 3. It currently awaits further deliberation in the House Rules Committee.
PAMPAC’s “Strengthening PAMPAC’s Political Muscle” Campaign is Back in Action
The campaign aims to build robust political engagement ahead of PAMED’s House of Delegates meeting in mid-October.
In an era of heightened polarization, PAMPAC remains firmly non-partisan, resisting pressure to “pick a side.” PAMPAC is already preparing for 2026, when the entire State House and half the State Senate will be up for reelection. Now is the time to build resources and momentum. Visit www.pamedsoc.org/PAMPAC to make a donation!




Berks County Medical Society member Vinti Shah, DO, received the inaugural Spirit of Reading Hospital Award at a Gala “Champions of Care” event at the DoubleTree in Reading on Thursday evening, September 11th.

Dr. Shah, who is married to current BCMS President Ankit Shah, MD, received the award from Reading Hospital President and CEO, and Past BCMS President, Charles Barbera, MD.

Vinti was recognized not only for her excellent work as the Division Chief of Hospice and Palliative Care at Reading Hospital, but especially for her compassionate care for patients and dedication to the well-being of her colleagues.

Congratulations Vinti from your many admiring colleagues!

of
18,
We are happy to make time for your patients
Eye Emergencies Cataracts
Glaucoma
Diabetic Eye Exams
Macular Degeneration
Macular Degeneration
Yes, we can see your patients same day for emergencies and often same week for consults.
Yes, we can see your patients same day for emergencies and often same week for consults.
At BERKS EYE PHYSICIANS AND SURGEONS, we are happy to offer state-of-the-art and efficient care. Our doctors provide appropriate diagnosis and treatment, and fast feedback to you. Whether
At BERKS EYE PHYSICIANS AND SURGEONS, we are happy to offer state-of-the-art and efficient care. Our doctors provide appropriate diagnosis and treatment, and fast feedback to you. Whether your patient has a sudden change in vision, cataracts, diabetes impacting vision, or even has a family history of glaucoma or macular degeneration, we would be honored to monitor and react to issues related to your patient’s eye health.
Domenic C. Izzo, Jr., MD, Benjamin Nicholas, MD, Francisco L. Tellez, MD, FACS, Michael C. Izzo, MD, Peter D. Calder, MD, Kasey L. Pierson, MD, Guri Bronner, MD