FP
MISSOURI FAMILY PHYSICIAN VOLUME 44, ISSUE 4

ISSUE INCLUDES: • MIDWEST OBESITY SYMPOSIUM HIGHLIGHTS • FAMILY MEDICINE MIXER MOMENTS • ANNUAL FALL CONFERENCE: WHAT TO EXPECT
AND MORE!




MISSOURI FAMILY PHYSICIAN VOLUME 44, ISSUE 4

ISSUE INCLUDES: • MIDWEST OBESITY SYMPOSIUM HIGHLIGHTS • FAMILY MEDICINE MIXER MOMENTS • ANNUAL FALL CONFERENCE: WHAT TO EXPECT
AND MORE!



MISSOURI FAMILY PHYSICIAN
EXECUTIVE COMMISSION
BOARD CHAIR Afsheen Patel, MD (Kansas City)
PRESIDENT Natalie Long, MD (Columbia)
PRESIDENT-ELECT Beth Rosemergey, DO, FAAFP (Kansas City)
VICE-PRESIDENT Lauren Wilfling, DO, FAAFP (St. Louis)
SECRETARY/TREASURER Lisa Mayes, DO (Macon)
DISTRICT 1 DIRECTOR Arihant Jain, MD, FAAFP (Cameron)
ALTERNATE Brad Garstang, MD (Kansas City)
DISTRICT 2 DIRECTOR Kelsey Davis-Humes, DO (Memphis)
ALTERNATE Robert Schneider, DO, FAAFP (Kirksville)
DISTRICT 3 DIRECTOR Christian Verry, MD (St. Louis)
DIRECTOR Kento Sonoda, MD, FAAFP (St. Louis)
ALTERNATE Stacy Jefferson, MD (St. Louis)
DISTRICT 4 DIRECTOR Vacant
ALTERNATE Jennifer Scheer, MD, FAAFP (Gerald)
DISTRICT 5 DIRECTOR Amanda Shipp, MD (Versailles)
ALTERNATE Jared James, MD, FAAFP (Jefferson City)
DISTRICT 6 DIRECTOR David Pulliam, DO, FAAFP (Higginsville)
ALTERNATE Misty Todd, MD (Sedalia)
DISTRICT 7 DIRECTOR Chad Byle, MD, FAAFP (Kansas City)
DIRECTOR Jacob Shepherd, MD, FAAFP (Lees Summit)
ALTERNATE R achel Hailey, MD, FAAFP (Lees Summit)
DISTRICT 8 DIRECTOR Andi Selby, DO, FAAFP (Branson)
ALTERNATE Barbara Miller, MD, FAAFP (Buffalo)
DISTRICT 9 DIRECTOR Douglas Crase, MD (Licking)
ALTERNATE Kristina Grant, DO (Houston)
DISTRICT 10 DIRECTOR Jenny Eichhorn, MD (Jackson)
ALTERNATE Vacant
DIRECTOR AT LARGE Eric Lesh, DO (Jackson)
RESIDENT DIRECTORS
Noah Brown, MD (Mercy)
Karstan Luchini, DO, MS (UMKC) – Alternate
STUDENT DIRECTORS
Taylor LaVelle (UMC)
Courtney Shubert (ATSU) – Alternate
AAFP DELEGATES
Peter Koopman, MD, FAAFP
Kate Lichtenberg, DO, FAAFP
Sarah Cole, DO, FAAFP (Alternate)
Jamie Ulbrich, MD, FAAFP (Alternate)
MAFP TEAM
EXECUTIVE DIRECTOR Bill Plank, CAE
MEMBER EXPERIENCE MANAGER Andrea Holloway, MA
MEMBER COMMUNICATIONS Brittany Bussey
The information contained in Missouri Family Physician is for informational purposes only. The Missouri Academy of Family Physicians assumes no liability or responsibility for any inaccurate, delayed, or incomplete information, nor for any actions taken in reliance thereon. The information contained has been provided by the individual/organization stated. The opinions expressed in each article are the opinions of its author(s) and do not necessarily reflect the opinion of MAFP. Therefore, Missouri Family Physician carries no respsonsibility for the opinion expressed thereon.
Missouri Academy of Family Physicians, 722 West High Street Jefferson City, MO 65101 • p. 573.635.0830 • f. 573.635.0148
Rooted in Purpose, Growing Together
A Complex Case of Shiga Toxin-Producing Escherichia coli (STEC) Infection in a 40-Year-Old Male with Multiple Comorbidities: A Diagnostic and Management Challenge
Neurological Recovery Following Correction of Vitamin B1 and Folate Deficiencies in a 38-Year-Old Male with Alcohol-Associated Cerebellar Ataxia and Peripheral Polyneuropathy
Long COVID: Demystifying a Condition You’re Already Treating
Externship Reflection
More Than Mixers: MAFP Brings Connection to Life in 2025
FHFM Silent Auction Fundraiser
Midwest Obesity Symposium: Learning Together, Caring Together
Advocacy Day
Members in the News
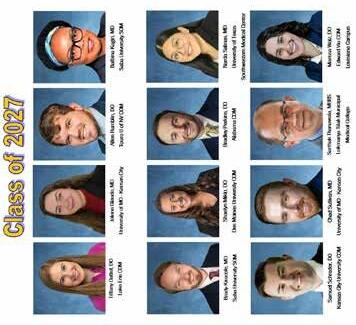
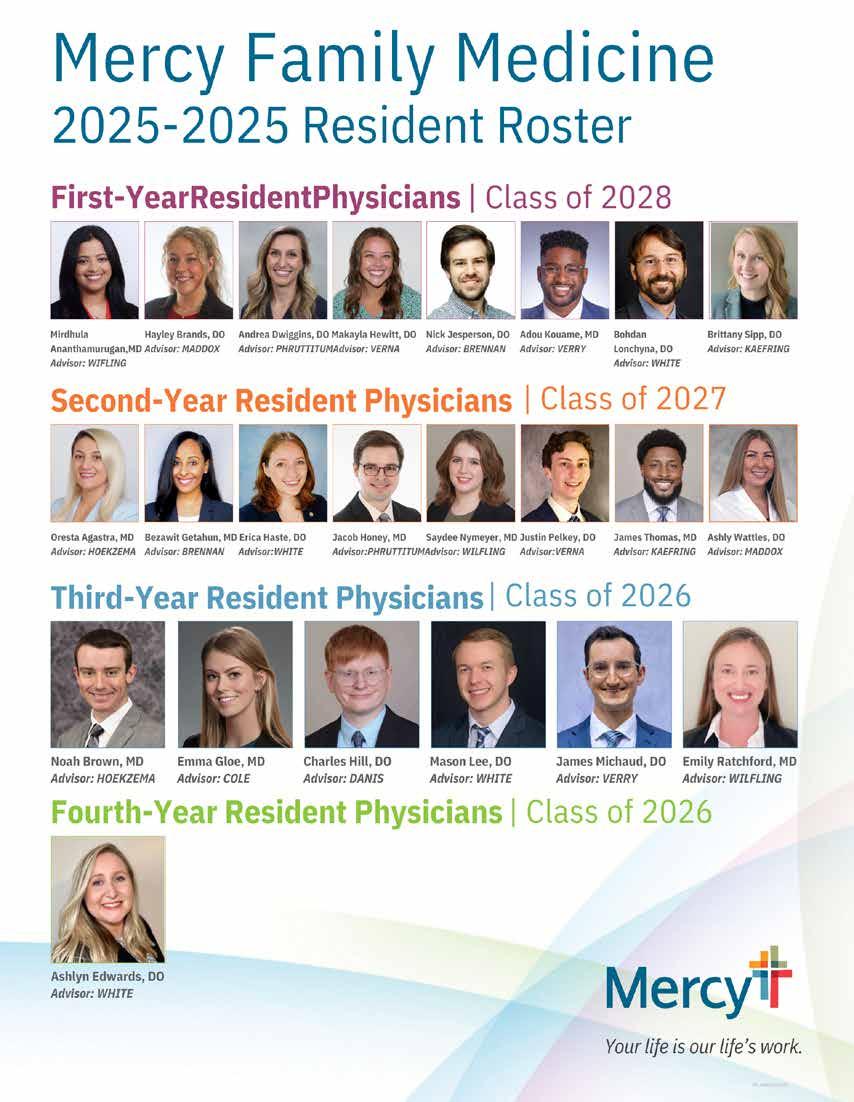
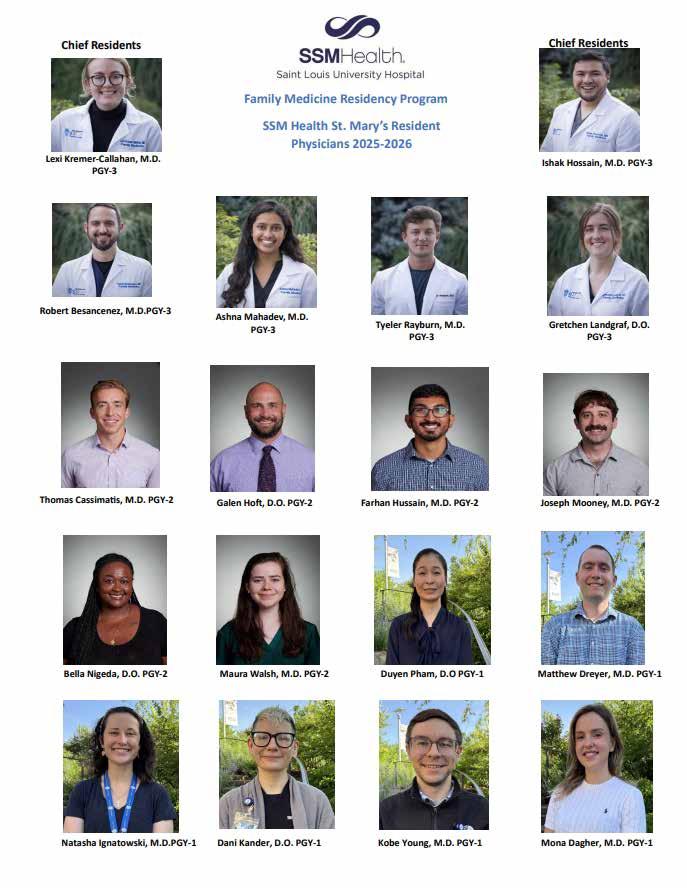
Resident Composites
Annual Fall Conference Schedule

Website: mo-afp.org • Email: office@mo-afp.org November 6-8, 2025 33rd Annual Fall Conference
InterContinental
Afsheen Patel, MD Board Chair
Kansas City, MO
When I first joined the Executive Commission, I wasn’t sure what to expect—but I knew exactly why I said yes.
Family medicine has always stood at the heart of community, connection, and continuity. Serving in a leadership role has only deepened my respect for the collective strength of Missouri’s family physicians—from new residents just finding their voice to seasoned doctors guiding with wisdom born of years in practice.
Stepping into this role felt, at times, like leaping into a fast-moving river. The challenges facing our profession are real: changing healthcare landscapes, workforce shortages, rising administrative burdens. But in every conversation, board or commission meeting, and conference, I was reminded that we are never swimming alone. Our Academy is powered by collaboration—a beautiful mix of generations, ideas, and shared purpose.
I saw firsthand how we show up for one another. We support the medical student deciding their future, the early-career physician learning to balance clinic with life, and the veteran doctor who still believes, after decades of service, that family medicine is the best specialty out there. We are stronger because of our differences, and united by our dedication to care, advocacy, and education.
One legacy I would like to leave is the initiation of a statewide obesity medicine program developed to raise awareness for elementary kids. I did not do this myself, but had two amazing elementary children work on this. The goal was to open doors to young inspiring family physicians who can reap the benefit of serving their community. I hope in the future we can encourage more initiatives led by young students to continue our legacy as family physicians. I also hope this resource will be beneficial to your community and we can make an impact to lessen the obesity epidemic.
As I close out my time as Board Chair, I leave feeling grateful, energized, and hopeful. This isn’t a goodbye—it’s simply a handoff in a relay that stretches across generations. And what an honor it has been to run this leg alongside you. We have worked tirelessly on preparing our board structure and ensuring we are ready for strategic planning in 2026. May the journey continue as we continue to ensure this organization can meet the needs of all our members.
OUR ACADEMY IS POWERED BY COLLABORATION— A BEAUTIFUL MIX OF GENERATIONS, IDEAS, AND SHARED PURPOSE.
In this role, I have had the privilege of witnessing a unique kind of leadership—quiet moments of mentorship, innovative ideas sparked during conference conversations, and fierce advocacy for our patients and profession. We are not just adapting to change; we are shaping it, together.
To our students, residents, physicians, and partners—thank you for trusting me, challenging me, and walking with me. Let’s continue building a future where family medicine thrives, together.
I would like to personally thank my mentors and colleagues through this journey. Kathy Pabst, who guided me along the way and is hopefully enjoying retirement. Bill, who we both joined this year with new challenges, and he has been exponential at leading this organization ahead. To Dr. Erika Ringdahl, my program director who believed in me all those years ago. Dr. Peter Koopman and Sara Cole, who have always been forthcoming with advice. Dr. Keith Ratcliff for his ever-mentoring personality- I promise we will never let you retire. The list would be endless as our organization has had amazing leadership in the past and continues to have young inspiring minds. Thank you all for this amazing journey.

Shiga toxin-producing Escherichia coli; hemolytic uremic syndrome; HIV; ulcerative colitis; gastrointestinal infection; case report
Shiga toxin-producing Escherichia coli (STEC) is an uncommon but potentially life-threatening cause of gastrointestinal illness, complicated by hemolytic uremic syndrome (HUS) in some cases. Patients with immunocompromising conditions and underlying gastrointestinal disease present unique diagnostic and therapeutic challenges.


We report a 40-year-old male with type 2 diabetes mellitus, hypertension, HIV, ulcerative colitis (UC), and a history of intravenous drug use. He presented with a 3-day history of abdominal pain, diarrhea, nausea, and vomiting. Initial evaluation at another facility suggested rhinovirus and possible pancreatitis. Persistent symptoms prompted further workup, revealing STEC infection. Management focused on supportive therapy, avoidance of antibiotics to mitigate HUS risk, and careful monitoring of UC activity.
This case illustrates the complexities of diagnosing and managing STEC in patients with multiple comorbidities, emphasizing the importance of multidisciplinary care, judicious antibiotic avoidance, and close follow-up to prevent complications.
Shiga toxin-producing Escherichia coli (STEC) is a rare but significant pathogen capable of causing severe gastrointestinal illness, with the potential to progress to hemolytic uremic syndrome (HUS). In adults, STEC is frequently associated with foodborne outbreaks, but transmission may also occur through sexual contact involving oral–anal exposure. Antibiotic therapy is generally contraindicated due to its association with increased HUS risk.
Patients with chronic gastrointestinal disease such as ulcerative colitis (UC) and immunocompromised states, including HIV infection, may present with overlapping symptoms, making diagnosis challenging. We present a case of STEC infection in a patient with multiple comorbidities and UC, highlighting diagnostic complexities and therapeutic considerations.
A 40-year-old male with a past medical history of:
• Type 2 diabetes mellitus (T2DM)
• Hypertension
• HIV infection on Biktarvy
• Ulcerative colitis (UC)
• Anxiety
• Cerebrovascular accident (CVA)
• Deep vein thrombosis (DVT)/pulmonary embolism (PE)
• History of endocarditis (2017, secondary to intravenous heroin use)
Sexually active with men; most recent encounter 7 days prior to presentation involving oral–anal contact.
Current vaping and marijuana use.
No alcohol use.
No pets at home.
Remote IV heroin use (last in 2017).
Allergies
Ancef, barium, coconut, Compazine, morphine, penicillin, Reglan, Zofran.
Initial presentation: Abdominal tenderness without peritoneal signs; afebrile; no hemodynamic instability.
Labs: Mild anemia; transient lipase elevation; normal renal function throughout course.
Imaging: Initial US suggested pancreatitis, but CT imaging was normal. No bowel obstruction or acute surgical pathology.
Endoscopy: UC-related mucosal changes on colon biopsy; gastritis on EGD.
The diagnosis of STEC was confirmed via stool PCR testing. Differential diagnoses included:
• UC flare
• Infectious colitis (bacterial, viral, parasitic)
• Pancreatitis (ruled out by CT)
• Viral gastroenteritis (initial rhinovirus diagnosis)
The persistence of symptoms, recent antibiotic exposure (doxycycline for STI treatment), and positive STEC PCR emphasized the need for cautious management without antibiotics to avoid precipitating HUS.
Supportive care: IV fluids, analgesia, antiemetics, gradual diet advancement.
Medication adjustments: Continued UC maintenance therapy; initiated PPI for gastritis.
Antibiotic avoidance: Based on Infectious Disease guidance due to HUS risk.
Multidisciplinary care: Gastroenterology and Infectious Disease consultations.
The patient improved with supportive measures and was discharged in stable condition. At follow-up, gastrointestinal symptoms had subsided, and there was no evidence of HUS or renal impairment. UC management was continued, and the patient was counseled on preventive measures to avoid enteric infections.
Date 2/14/25
2/15/25
2/16/25
2/18/25
3/1/25
3/4/25
3/6/25
First ED visit (Missouri Baptist Medical Center): Diagnosed with rhinovirus; abdominal US suggested pancreatitis; discharged with supportive care.
Second ED visit (St. Luke’s Des Peres Hospital): Persistent GI symptoms; labs – Hgb 10.9 g/dL, lipase 839 U/L; CT abdomen normal. Admitted for evaluation.
Lipase decreased to 293 U/L; GI PCR positive for STEC. Antibiotics withheld per Infectious Disease recommendations. Supportive therapy initiated.
Gradual improvement; discharged with outpatient follow-up.
Readmission for abdominal pain, hematochezia. Labs – ESR 47 mm/hr, ALT 72 U/L; CT abdomen: mild gallbladder distention, no obstruction.
Colonoscopy: Internal hemorrhoids, otherwise normal mucosa; biopsies – focal crypt distortion, lymphoid nodules (consistent with UC inflammation).
EGD: Gastritis; biopsies negative for H. pylori. Started on a proton pump inhibitor (PPI) for 8 weeks.
This case illustrates the complexity of diagnosing and managing STEC infection in patients with multiple comorbidities, particularly those with HIV and chronic gastrointestinal disease.
STEC infection can be transmitted via contaminated food or sexual contact involving fecal–oral exposure. The hallmark of management is supportive therapy, with antibiotics generally avoided to prevent HUS—a complication that is particularly concerning in immunocompromised hosts.
In our patient, the coexistence of UC and STEC created diagnostic uncertainty, as both can cause hematochezia and abdominal pain. Colonoscopic findings of focal crypt distortion and lymphoid hyperplasia were consistent with UC rather than acute infectious colitis, although STEC likely precipitated the symptomatic flare.
Early Infectious Disease involvement was critical in guiding
• Differentiate infectious colitis from IBD flare through a combination of stool PCR, endoscopic evaluation, and histology.
• Multidisciplinary care is essential for managing STEC in patients with complex medical histories.
• Maintain vigilance for HUS, even in patients who initially appear stable.
1. Hunt JM. Shiga toxin-producing Escherichia coli (STEC). Clin Lab Med. 2010 Mar;30(1):21-45. doi: 10.1016/j.cll.2009.11.001. PMID: 20513540; PMCID: PMC7126671.
2. Serlin MH, Dieterich D. Gastrointestinal Disorders in HIV. Global HIV/AIDS Medicine. 2008:251–60. doi: 10.1016/B978-1-41602882-6.50027-7. Epub 2009 May 15. PMCID: PMC7173545.
3. New York State Department of Health. (2017, August). Shiga toxin-producing E. coli (STEC) infections – Fact sheet. https://


Missouri Academy of Family Physicians Political Act ion Committee
small donations make a big difference
To make a donation, scan the QR code or visit moafp.formstack.com/forms/mafp_pac_donation_form. Learn more about the MAFP PAC by visiting www.mo-afp.org/advocacy/political-action-committee.


Chronic alcohol use is associated with nutritional deficiencies, particularly thiamine and folate, which can lead to severe neurological complications. Early recognition and correction are vital to prevent permanent disability.
We present a 38-year-old male with alcohol dependence who developed progressive cerebellar ataxia and peripheral neuropathy, resulting in wheelchair dependence. Laboratory studies revealed severe thiamine and folate deficiencies with macrocytosis and hyperhomocysteinemia.
The patient was treated with high-dose parenteral thiamine, oral folic acid, a multivitamin regimen, and vitamin D supplementation. He received neuropathic pain management, psychiatric support for alcohol cessation, and intensive physical and occupational therapy.
Over six months, the patient showed significant neurological recovery, transitioning from wheelchair to walker ambulation, with normalization of vitamin levels and improved nerve conduction studies.
This case underscores the importance of prompt recognition and correction of vitamin B1 and folate deficiencies in alcohol-associated neurological disorders. A multidisciplinary approach combining nutritional repletion, rehabilitation, and psychiatric support can yield substantial functional recovery.
Chronic alcohol use is strongly associated with nutritional deficiencies, particularly thiamine and folate, which are essential for neuronal metabolism. Thiamine deficiency is implicated in Wernicke–Korsakoff syndrome, alcoholic cerebellar degeneration, and alcoholic peripheral neuropathy¹. Folate deficiency also contributes to neuropathy and myelopathy, especially when combined with cobalamin deficiency². Deficiencies can lead to cerebellar degeneration, polyneuropathy, and cognitive dysfunction if unrecognized. Prompt recognition and supplementation are critical to prevent permanent neurological damage³.
Alcohol-related cerebellar ataxia typically results from selective atrophy of the anterior cerebellar vermis. Prolonged abstinence has been associated with improved gait and balance, and sometimes partial reversal of vermian atrophy⁴. Alcoholic polyneuropathy, affecting up to 46% of chronic drinkers, is a length-dependent axonal neuropathy due to combined alcohol toxicity and vitamin deficiencies⁵. Early disease can improve substantially with abstinence and supplementation, while advanced axonal loss often leaves residual disability⁶.
Patient Information: A 38-year-old man with a history of alcohol dependence, hypothyroidism, and depression presented to primary care in September 2024, two days after abruptly stopping alcohol. He reported progressive distal limb weakness, gait instability, tremors, and bilateral neuropathic pain, resulting in wheelchair dependence.
Clinical Findings: He appeared tremulous and malnourished. Neurologic exam showed a wide-based gait that he could not perform without support, impaired heel–knee–shin coordination consistent with cerebellar ataxia, fine postural tremor, mild distal lower-extremity weakness, diminished ankle reflexes, and stocking-glove sensory loss. Cognition and eye movements were intact.
Investigations: Laboratory testing revealed thiamine 34.5 nmol/L (low), folate <2.0 ng/mL (severely low), pyridoxine 13.7 nmol/L (borderline), MCV 105 fL, and homocysteine 130.1 μmol/L. Brain MRI showed cerebellar vermian atrophy without acute lesions. EMG/NCS demonstrated chronic axonal sensorimotor polyneuropathy without active denervation.
High-dose parenteral thiamine (e.g., 500 mg IV daily for 3 days, then weekly) was initiated promptly, followed by oral thiamine 100 mg twice daily. Folic acid 1 mg daily and a high-potency multivitamin were started, with vitamin D supplementation. Gabapentin, later transitioned to pregabalin, was prescribed for neuropathic pain. Psychiatric medications included quetiapine and amitriptyline. He engaged in structured alcohol-recovery counseling and remained abstinent.
Physical therapy progressed from assisted range-of-motion and strengthening exercises to gait training with a walker. Occupational therapy addressed tremor and coordination. Nutritional counseling emphasized protein-rich, calorie-adequate meals with sustained B-vitamin intake.
At 3 months, neuropathic pain diminished and he transitioned from wheelchair to walker; vitamin levels normalized. At 6 months, homocysteine fell to <20 μmol/L, and EMG/NCS showed mild
improvements in conduction. He ambulated ~100 meters with a walker, with residual balance and proprioceptive deficits.
This case demonstrates substantial recovery of alcohol-related neurological deficits when thiamine and folate deficiencies are corrected and abstinence is maintained. Thiamine deficiency disrupts neuronal glucose metabolism, with preferential injury to cerebellar Purkinje cells and peripheral axons¹. Folate deficiency leads to demyelination and elevated homocysteine, compounding neurotoxicity². Recovery depends on whether injury is metabolic and reversible versus structural and irreversible. The absence of active denervation suggested potential for functional recovery once metabolic deficits were corrected. Similar cases highlight reversibility with aggressive vitamin repletion and abstinence³⁴⁶. Multidisciplinary management, including psychiatric and physical rehabilitation, is essential for optimal outcomes.
In alcohol-dependent patients with neurologic deficits, early identification and correction of thiamine and folate deficiencies are crucial. With comprehensive multidisciplinary care, including vitamin repletion, rehabilitation, and psychiatric support for sustained abstinence, even severe alcohol-related cerebellar ataxia and polyneuropathy can show meaningful recovery.
1. Praharaj SK, Munoli RN, Shenoy S, Udupa ST, Thomas LS. Highdose thiamine strategy in Wernicke–Korsakoff syndrome and related thiamine deficiency conditions associated with alcohol use disorder. Indian J Psychiatry. 2021;63(2):121-6.
2. Koike H, Nakamura T, Ikeda S, Takahashi M, Kawagashira Y, Iijima M, et al. Alcoholic myelopathy and nutritional deficiency. Intern Med. 2017;56(1):105-8.
3. Paparrigopoulos T, Tzavellas E, Karaiskos D, Kouzoupis A, Liappas I. Complete recovery from undertreated Wernicke–Korsakoff syndrome following aggressive thiamine treatment. In Vivo. 2010;24(2):231-3.
4. Proudfoot M, Wilkins A. Treatment of cerebellar ataxia in the context of systemic diseases. Curr Treat Options Neurol. 2017;19(12):47.
5. Mellion M, Gilchrist JM, de la Monte SM. Alcohol-related peripheral neuropathy: nutritional, toxic, or both? Muscle Nerve. 2011;43(3):309-16.
6. Peters TJ, Kotowicz J, Nyka W, et al. Treatment of alcoholic polyneuropathy with vitamin B complex: a randomized controlled trial. Alcohol Alcohol. 2006;41(6):636-42.
7. Chopra K, Tiwari V. Alcoholic neuropathy: possible mechanisms and future treatment possibilities. Br J Clin Pharmacol. 2012;73(3):348-62.
8. Assaker R, et al. I drank too much and now I can’t walk: a case of alcohol-induced dysautonomia. Oxf Med Case Rep. 2021;2021(8):omab072.

Abby L Cheng, MD, MPHS Washington
University St. Louis, MO

Stephen Cohen, MD Primary Care, BJC Medical Group
St. Louis, MO
Long COVID is defined as the presence of new or worsened symptoms that persist at least three months after a SARS-CoV-2 infection.1 Multiple pathophysiologic mechanisms are responsible for Long COVID symptoms, including persistent viral reservoirs in tissues, immune dysregulation, mitochondrial dysfunction, endothelial inflammation, and microbiome changes, among others.2,3
Although the COVID-19 pandemic ended in 2023, approximately 13 million adults and nearly 300,000 children and adolescents in the US continue to experience Long COVID. This equates to 1 in 20 adults and 1 in 250 children and adolescents.4,5 Furthermore, new Long COVID cases continue to occur, although at a lower incidence than during the pandemic.4 These statistics suggest that essentially every family practice and primary care physician is already managing at least some patients who are living with Long COVID. Physicians need to feel equipped to recognize and diagnose Long COVID because some aspects of Long COVID management do not follow traditional supportive care practices and because medical and social
resources are available for people with Long COVID.
Long COVID should be included on the differential diagnosis for any patient who has new or worsened symptoms of unclear etiology for three months or longer since the COVID-19 pandemic.6 Common Long COVID symptoms include exaggerated fatigue, post-exertional malaise (i.e., energy “crashes” after physical, mental, or emotional activity), memory and attention impairment (often called “brain fog”), orthostasis and palpitations (from dysautonomia), myalgias and neuropathic pain, smell and taste changes, gastrointestinal upset, and sleep dysfunction. Any person can develop Long COVID, but it is more common among people who are female, have underlying health conditions (e.g., obesity, cardiovascular disease, respiratory conditions, diabetes), have not received COVID-19 vaccines, and/or had severe acute COVID-19 symptoms.6 Diagnosing Long COVID can be challenging because there is currently no clinically
available diagnostic test to confirm or rule out the diagnosis and because the preceding acute SARS-CoV-2 infection may have been asymptomatic or mild. As such, Long COVID is a clinical diagnosis, and a positive SARS-CoV-2 test or a preceding symptomatic upper respiratory infection is not required to diagnose Long COVID.1
Even when the diagnosis of Long COVID is strongly suspected, it is important to consider, diagnose, and address any competing or coexisting conditions because Long COVID can “unmask” or exacerbate previously subclinical conditions. Therefore, even though Long COVID can cause debilitating symptoms despite normal results on common blood and imaging tests, basic bloodwork such as a complete blood count (CBC), comprehensive metabolic panel (CMP), thyroid studies, and potentially inflammatory markers and vitamin D, B1, and B12 levels should be considered during the diagnostic workup for Long COVID to rule out coexisting, often modifiable, conditions (e.g., Wernicke encephalopathy or beriberi due to malnutrition or malabsorption).6 Additional laboratory and imaging studies should also be performed, as indicated based on the patient’s presenting symptoms (e.g., chest radiograph for cardiopulmonary symptoms, ferritin and iron panel for physical fatigue).
When the diagnosis of Long COVID is suspected, an important initial step is to acknowledge and validate the patient’s experience because many people with Long COVID have suffered secondary harm from being dismissed by loved ones and even healthcare team members as imagining symptoms, exaggerating symptoms, or merely experiencing physical manifestations of stress, depression, or anxiety. Example phrases to provide validation and education include: “The diagnosis of Long COVID fits with your symptoms. Many patients with Long COVID, though not all, improve or fully recover over several months or even years. Although we don’t have a cure right now, many patients can manage their symptoms and improve their quality of life with the treatment strategies we do have. Researchers are learning more about Long COVID every day and are working to identify effective treatments.”6
Medical treatment of Long COVID symptoms largely mirrors symptom-based management that occurs outside the context of Long COVID, with one important exception. Specifically, patients should not be encouraged to push through fatigue, pain, or other symptoms that are exacerbated after (rather than during) activity. These “crashes” are called post-exertional malaise (PEM) or post-exertional symptom exacerbation (PESE). Myopathic changes and mitochondrial damage occur during these crashes, and pushing through the symptoms can cause lasting muscle damage and a prolonged setback in activity tolerance.3 Rather, patients should be counseled to manage their symptom triggers with pacing and energy conservation strategies, such as by spreading out energy-expending activities across the day and week, scheduling rest breaks, and modifying activities to conserve physical and mental energy (e.g., sit down while showering or chopping vegetables, push or slide objects instead of lifting them, limit background noise and interruptions during cognitive work, etc.). Physical, occupational, and/or speech therapists who have experience treating dysautonomia, PEM/PESE, and/or cognitive impairment can significantly assist patients in improving their overall function and quality of life. Work accommodations and/or disability leave are also warranted and extremely helpful for some adult patients. Optimizing a person’s lifestyle habits such as sleep hygiene, adequate hydration, proper nutrient intake, etc., can also result in tangible improvements in function.
No medications are FDA-approved specifically for Long COVID yet. Rather, pharmacologic management of Long COVID currently consists primarily of medications that primary care physicians are experienced in prescribing, such as beta blockers for dysautonomia,
stimulants for brain fog, and tricyclic antidepressants for sleep, mood, and neuropathic pain, among others. A printable table of additional medication options is available at LongCOVID-STL.org (see QR code). In the context of Long COVID, medication changes should be made particularly slowly and under close monitoring. Medications may improve some Long COVID symptoms while exacerbating others (e.g., propranolol may improve dysautonomia but worsen fatigue), and medication deprescribing should be thoughtfully considered because some medications which were previously tolerated by a patient may not be tolerated anymore.6
Long COVID symptoms can improve and then recur, especially due to stressors such as a recurrent SARS-CoV-2 infection. As such, the COVID-19 vaccine and boosters are generally encouraged for people with Long COVID. Although the vaccine has been associated with temporary symptom flares in some patients, population level data repeatedly demonstrate that COVID-19 vaccination reduces a person’s risk of Long COVID symptoms, and each additional booster reduces the risk even further.7
Long COVID manifests differently across the age spectrum and is more common among adolescents than younger aged children.8 In preschool-aged children and younger, the most common symptoms include a cough, trouble sleeping, and/or daytime tiredness and low energy. Infants and toddlers can also experience a persistently stuffy nose and/or poor appetite. In school-aged children, Long COVID commonly presents as trouble with memory or focus, lightheadedness or dizziness (i.e., dysautonomia), and headaches or other pain. Preadolescents may also have skin itchiness or rash, nausea or vomiting, trouble sleeping, and/or new phobias or school avoidance. In contrast, adolescents more commonly experience smell/taste changes, low energy, and tiredness after walking (i.e., PEM/PESE).5
Symptom-specific school accommodations may be warranted, with the goal of tapering accommodations if/as symptoms improve. Example accommodations include: extra time to walk between classes, use of the elevator instead of the stairs, increased test taking time, reduced homework volume, and scheduled rest breaks.9
For practical point-of-care clinical guidance, clinicians can reference a table-based compendium guidance statement which was published in 2025 by the American Academy of Physical Medicine and Rehabilitation (AAPM&R) Long COVID Collaborative. This guidance statement was designed for primary care and other clinicians who are inevitably providing front-line assessment and management of Long COVID within the context of an already busy clinical practice. A freely downloadable version of the guidance tables is available at LongCOVID-STL.org (see QR code).6 Much of the guidance in this statement is also applicable for patients with other infection-associated chronic conditions such as myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS).

Additionally, through a federal grant, organizations including Washington University in St. Louis, the University of Missouri, and the St. Louis Integrated Health Network created the St. Louis Long COVID Initiative.10 The Initiative’s LongCOVID-STL.org website details additional clinical efficiency tools, as well as referral instructions for regional medical and rehabilitation clinics with experience addressing
Long COVID. Example efficiency tools include a link to the AAPM&R guidance statement, quick tips to support patients applying for disability, templates for notes and rehabilitation referrals, and more. A unique referral option is group-based, telehealth rehabilitation for patients who face barriers to accessing traditional one-on-one physical, occupational, or speech therapy for Long COVID (e.g., due to underinsurance or geographic distance to therapists who are comfortable treating Long COVID symptoms). This group-based rehabilitation is covered by Medicaid and is available via referral to the Washington University Living Well Center. The Initiative also delivers Long COVID presentations for primary care teams through the ShowMe ECHO program and through invited presentations by interested health centers. Prior ECHO presentations are recorded and freely available.11
The patient-facing section of the St. Louis Long COVID Initiative’s LongCOVID-STL.org website includes general information about Long COVID, self-management strategies, flyers for regional Long COVID research studies, and contact information for the Initiative’s community health worker, whom patients can directly contact for assistance navigating medical and social support resources. The Initiative also hosts peer support groups, and it ensures timely clinic appointments with a behavioral health counselor for people with Long COVID.
• Consider Long COVID on the differential diagnosis for any persistent, unexplained symptoms.
• Consider and address coexisting conditions.
• Provide supportive care for Long COVID symptoms.
• Recommend pacing and energy conservation for patients with energy “crashes.”
• Incorporate Long COVID clinical efficiency tools into clinical practice. (LongCOVID-STL.org, AAPM&R compendium guidance tables6)
• Refer patients to regional resources as needed. (LongCOVID-STL. org)
• Watch for emerging Long COVID diagnostic tools and therapeutics in coming years.12
1. National Academies of Sciences E, Medicine. A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences. The National Academies Press; 2024:186.
2. Al-Aly Z, Davis H, McCorkell L, et al. Long COVID science, research and policy. Nat Med. 2024/08/09 2024;doi:10.1038/s41591-02403173-6
3. Appelman B, Charlton BT, Goulding RP, et al. Muscle abnormalities worsen after post-exertional malaise in long COVID. Nat Commun. Jan 4 2024;15(1):17. doi:10.1038/s41467-023-44432-3
4. U.S. Census Bureau, Household Pulse Survey, 2022–2024. Long COVID. National Center for Health Statistics. Updated October 3, 2024. Accessed March 12, 2025, https://www.cdc.gov/nchs/ covid19/pulse/long-covid.htm
5. Gross RS, Thaweethai T, Salisbury AL, et al. Characterizing Long COVID Symptoms During Early Childhood. JAMA Pediatr. May 27 2025;doi:10.1001/jamapediatrics.2025.1066
6. Cheng AL, Herman E, Abramoff B, et al. Multidisciplinary collaborative guidance on the assessment and treatment of patients with Long COVID: A compendium statement. PM & R : the journal of injury, function, and rehabilitation. Jun 2025;17(6):684-708. doi:10.1002/pmrj.13397
7. Hedberg P, van der Werff SD, Nauclér P. The Effect of COVID-19 Vaccination on the Risk of Persistent Post-COVID-19 Condition: Cohort Study. J Infect Dis. Jun 2 2025;231(5):e941-e944. doi:10.1093/infdis/jiaf133
8. Ford ND, Vahratian A, Pratt CQ, Yousaf AR, Gregory CO, Saydah S. Long COVID Prevalence and Associated Activity Limitation in US Children. JAMA Pediatr. Feb 3 2025;doi:10.1001/ jamapediatrics.2024.6206
9. Malone LA, Morrow A, Chen Y, et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of postacute sequelae of SARS-CoV-2 infection (PASC) in children and adolescents. PM & R : the journal of injury, function, and rehabilitation. Oct 2022;14(10):1241-1269. doi:10.1002/pmrj.12890
10.The St. Louis Long COVID Initiative. Agency for Healthcare Research and Quality. https://www.ahrq.gov/sites/default/ files/wysiwyg/coronavirus/long-covid-care-network/wu-stlouisgrantee-profile.pdf
11.Long-COVID Special ECHO Sessions. University of Missouri. Accessed March 28, 2025, https://showmeecho.org/special-echosessions/
12.RECOVER: Researching COVID to Enhance Recovery. National Institutes of Health. Accessed July 7, 2025, 2025. RecoverCOVID. org

Real data that provides information such as salary, satisfaction, benefits and job titles is vital when negotiating a contract, considering a job offer and even just planning your career. That’s what the AAFP Career Benchmark Dashboard has been doing since 2023—and now it’s time to fuel the dashboard with the latest data.
The Missouri Academy of Family Physicians urges you to take 10 minutes to fill in your information—anonymously of course. The more people who fill it out, the richer the dashboard becomes with insights for you and your peers from all over the United States.
Once the 2025 data is in, you’ll be able to filter the information to compare 2023 to 2025 numbers, as well as all the other perimeters currently available on the dashboard. Plus, this year’s survey will include questions that cover direct primary care and obstetrical care.
Now’s the time to know your worth! Fill out this year’s survey and encourage your colleagues to do the same to create a robust, powerful tool.
Any family physician can take the anonymous survey through November 3, 2025.

Learn more: https://www.aafp.org/familyphysician/practice-and-career/managing-yourcareer/family-medicine-career-benchmarkdashboard.html.

Katelyn Junghans, MS I
UMKC School of Medicine - Kansas City
Site: Mercy Family Medicine Residency - St. Louis
Gratitude hardly begins to capture how thankful I am to the MAFP and Mercy Family Medicine Residency for the opportunity to participate in the Family Medicine Externship Program. Throughout this experience, I developed my medical knowledge, enhanced patient interactions, and refined my advocacy skills. Most importantly, I was privileged to witness and be part of a clinical team that cared deeply for not only their patients but also for one another and their community.
As a rising second-year medical student, my clinical experience before this externship had been limited to a weekly continuity clinic. Having the chance to engage in hands-on learning so early in my training helped me translate concepts from the classroom into clinical application. I am especially grateful to the residents and attending physicians who took time to answer my many questions and guide me along the way. My rotation experiences, which spanned inpatient care, outpatient clinics, procedures, sports medicine, women’s health, and osteopathic manipulation, provided me with a meaningful glimpse into the breadth of family medicine. I even had the opportunity to begin learning the fundamentals of POCUS.
The culture at Mercy was evident from the very first day. The way residents and attendings supported one another created a truly uplifting environment that extended naturally to patient care. The positive rapport with patients was remarkable, and I learned how something as simple as an introductory handshake and intentional listening can foster trust and make patients feel genuinely cared for.
A highlight of the externship was the focus on advocacy. I completed the Society of Teachers of Family Medicine Advocacy Course, utilized the AAFP advocacy template, and conducted a community needs assessment. My capstone project centered on reducing barriers to cervical cancer screening, a topic that underscored the vital role family physicians play in advancing both individual and public health.
Finally, I want to express my sincere thanks to the many team members I was fortunate to learn from: Dr. Cole, Dr. White, Dr. Brennan, Dr. Phrittitum, Dr. Verry, Dr. Brown, Dr. Gloe, Dr. Michaud, Dr. Pelkey, and Dr. Wattles, Ashley, and Holly. Thank you for welcoming me, teaching me, and sharing your passion for family medicine.
Humza Rehman, MS I
Saint Louis University School of Medicine
Site: Freeman Family Medicine Residency
Over the course of my one-month family medicine externship in Joplin and Neosho, Missouri, I was exposed to a broad range of clinical experiences and patient populations that deepened my understanding of primary care. The externship not only sharpened my clinical lens but also gave me a more nuanced view of the social and interpersonal dimensions of medicine—especially in community-based and rural settings.
In Joplin, I encountered a wide array of common conditions frequently managed in family medicine, including urinary tract infections, musculoskeletal pain, seasonal allergies, and mental health conditions such as depression. I observed episodes of presyncope due to orthostatic hypotension and worked with providers who routinely managed complex chronic illnesses like hypertension, COPD, and acute kidney injury. One day, I observed a
patient with persistent fatigue and shortness of breath—symptoms that prompted a thorough evaluation, eventually revealing early-stage COPD. I was struck by how the resident explained the diagnosis and collaborated with the patient to build a realistic and sustainable care plan.
Neosho offered a slightly different experience, highlighting some of the unique challenges in more rural and underserved communities. One case that stood out involved a young child with bacterial conjunctivitis whose parents had delayed care due to insurance and transportation issues. It reminded me of the systemic barriers many families face just to access basic healthcare. I also observed joint injections and cryotherapy, which broadened my appreciation for the procedural scope of family medicine.
Each day, I shadowed a different physician or resident, which gave me a rich selection of perspectives. While I primarily worked alongside residents, I also had the opportunity to observe Dr. De’Mour and Dr. Miller. Each provider approached patient care with their own distinctive style—some more formal, others more conversational—but all shared a common thread of humility and respect toward their patients. I was especially impacted by how residents navigated clinical uncertainty with openness, often framing their conversations with patients as a collaborative process: “Let’s figure this out together.” This mindset not only created trust but also modeled a kind of medicine that felt deeply human.
In addition to clinical experiences, our externship included weekly didactic sessions led by residents. These sessions were a valuable opportunity to deepen our understanding of both
common and complex topics in family medicine. We reviewed journal articles and discussed current guidelines and challenges in treating conditions such as alcohol use disorder, substance use disorder in adults, and depression in children and adolescents. Each session also included resident-led case presentations, which highlighted unique diagnostic dilemmas and reinforced the importance of evidence-based decision-making in primary care. Throughout the externship, I grew in both confidence and perspective. I began to understand that family medicine isn’t just about managing chronic disease or diagnosing acute illness—it’s about building long-term, trust-based relationships in which the physician becomes a steady presence in a patient’s life. I learned that listening, empathy, and follow-through are often more powerful than any prescription.
One particularly memorable moment came in Neosho, when a patient who had been struggling with anxiety and insomnia for months returned for follow-up. After trying a new treatment plan and implementing sleep hygiene recommendations, he thanked the team and said, “This is the first time I’ve felt like myself in years.” That brief encounter reinforced why continuity and compassion are so critical in primary care. This experience affirmed my interest in family medicine and opened my eyes to the vital role of community physicians. I could absolutely see myself practicing in a similar setting—one where long-term care, patient relationships, and community involvement form the heart of clinical work.
Join us for the Missouri Academy of Family Physicians Annual Meeting, held in conjunction with the 33rd Annual Fall Conference on November 7 at the InterContinental Kansas City at the Plaza. This meeting is open to all MAFP members.
During the meeting, members will vote on proposed Bylaws revisions. You can review the updated MAFP Bylaws in advance by visiting https://www.mo-afp.org/wp-content/ uploads/MAFP-BYLAWS-11-2025-FINAL.pdf.
If you haven’t registered yet, don’t wait.
Join us on November 7–8 in Kansas City for a weekend filled with learning, connection, and celebration with your family medicine colleagues.


Family physicians spend their days caring for others, but in 2025 the Missouri Academy of Family Physicians (MAFP) made sure its members had time to care for themselves and each other. Through a series of Family Medicine Mixers, MAFP gave members a chance to step away from the clinic, connect with colleagues, and experience the joy of being part of a vibrant, statewide family medicine community.
At its core, MAFP exists to support, connect, and advocate for Missouri’s family physicians. These mixers are a living example of that mission. They provide space for members to share ideas, strengthen relationships, and recharge, reminding everyone that medicine is more than work—it’s about community.
Attendees repeatedly shared that the mixers helped them feel seen, valued, and part of something bigger. Those who missed out? They’ll be marking their calendars early next year after hearing the buzz.
Kansas City Mixer – Chicken N Pickle (August 21, 2025):
A summer evening full of laughter, pickleball, and friendly rivalries. Whether on the courts or at the tables, members walked away with new friendships, stronger bonds, and staying out of the kitchen.
Columbia Mixer – Back 2 Basics Cooking Class (August 28, 2025):
A night of teamwork, great food, and even better company. Members swapped lab coats for aprons, proving that when physicians cook together, connections grow deeper.
St. Louis Mixer – Zoo After Hours Tour (September 4, 2025):
A magical evening surrounded by animals, laughter, and familyfriendly fun. Members connected with colleagues while exploring the zoo after dark—a purrfect experience you had to be there to believe, oh my!
The mixers weren’t just events—they were experiences that created lasting memories and strengthened the heartbeat of Missouri’s family medicine community. For those who joined us, the connections are still sparking new friendships, building stronger bonds, collaborations, and joy. For those who didn’t, the message is clear: you don’t want to miss the next MAFP Event.
MAFP will continue creating these opportunities because our members are the meaning of MAFP. We exist to celebrate you, support you, and connect you—not only in the clinic, but beyond it.
So next time you see an invitation to a Family Medicine Mixer, Annual Fall Conference, Advocacy Day, etc., remember this is more than a social hour. It’s a chance to laugh, learn, and live out the spirit of family medicine together.








The Family Health Foundation of Missouri (FHFM) supports medical students and family medicine residents’ leadership development through participation in national and state conferences. We need your help to support these programs.
The FHFM will hold an auction during the Annual Fall Conference on November 7-8, 2025, at InterContinental on the Plaza in Kansas City, MO. Auction items will be available at the conference and on a virtual platform for those unable to attend our annual gathering.
With a goal of raising $5,000, the FHFM is counting on your generosity to help fund its scholarship program and leadership development for residents and medical students. The deadline to submit a donation form is October 25. Please send photos of donated items to be included on our virtual auction site. However, all donations can be received through November 1st (unless they are delivered to the conference).
Here are some items to consider, but not limited to:
• Anything local that represents your hometown / area
• Art and handmade goods (especially if made by a family physician or their family)
• Athletic tickets and gear
• Celebrity or team-autographed items
• “Of the Month” Gifts (wine, fruit, cookies, etc.)
• Performance tickets (theater, music, etc.)
• Restaurant certificates
• Subscriptions
• Theme baskets
• Trips and weekends (lake houses, resorts, condos, houseboats, etc.)
• Unique experiences and travel



On September 12–13, 2025, Hermann, Missouri became more than just a picturesque town with vineyards and history—it transformed into the hub of connection, education, and inspiration during the very first Midwest Obesity Symposium.
Physicians, health professionals, and advocates gathered not just to learn, but to truly connect. This wasn’t your typical “sit quietly and take notes” conference—it was alive with conversation, laughter, and the spirit of unity. From the opening remarks to the closing session, the atmosphere buzzed with excitement, purpose, and a shared commitment to better patient care.
The Symposium highlighted what happens when professionals from across the region come together. Attendees discovered new perspectives, shared strategies, and built partnerships that will outlast the weekend. Tackling obesity medicine is no small feat, but it becomes lighter and more achievable when approached as a team.
Between learning sessions, attendees found time to breathe, stretch, and reset. Yoga sessions, mindfulness breaks, and moments of reflection reminded us that caring for patients starts with caring for ourselves. The balance of education and restoration made the experience both energizing and memorable.


Our incredible speakers shared cutting-edge knowledge, practical strategies, and compassionate approaches—all focused on improving the care of patients living with obesity. Attendees returned to their practices with tools, resources, and renewed motivation to make meaningful differences in their patients’ lives.
The Symposium wasn’t all work—there was plenty of fun woven throughout. From the Friday night dinner outing to the winery tour, to those early-morning yoga mats bravely unrolled, the event reminded us of that laughter, joy, and shared experiences are powerful tools for connection.
The Midwest Obesity Symposium was more than a conference—it was a movement of unity, learning, and joy. Together, we proved that when care meets connection, patients win.

The next big event, MAFP’s Scientific CME, will be held on August 28–29, 2026. The topic is still TBD—but keep an eye on the MAFP website and communications for announcements. You won’t want to miss it!






MONDAY, FEBRUARY 23
8:00 am - 4:00 pm – Advocacy 101 for New Advocates (including students and residents)
6:00 - 8:30 pm – Virtual Advocacy Review
TUESDAY, FEBRUARY 24
8:00 - 9:00 am – Breakfast Buffet at Courtyard Marriott 9:00 am - 4:00 pm – Legislator Appointments

We encourage you to invite a colleague, medical student, or resident to join you to promote the importance of family medicine and primary care. This is your opportunity to educate your State Senator and State Representative on issues that affect you, your profession, and your patients.
Make your lodging reservation at the Courtyard Marriott, 610 Bolivar Street, Jefferson City, MO 65101, (573) 761-1400. Be sure to reference the Missouri Academy of Family Physicians to receive the discounted rate of $134 per night. The last day to make a reservation in our block is January 2, 2026. Any reservations made after that date are subject to availability.
(573) 635-0830 or emailing office@mo-afp.org.
Affinia Healthcare has been awarded a grant from the State of Missouri, through the Department of Health and Senior Services, that provides $333,000 per year for three years — totaling $1,000,000 — to support the continued development of the newly formed Family Medicine Residency Program.
This new program is part of the Missouri Graduate Medical Education Grant Program, which was created to address the shortage of physicians in our state—especially in rural and underserved areas. By expanding residency opportunities in Missouri, the program aims to train and retain more doctors who are committed to caring for the communities that need them most.

The Family Medicine Residency Program will prepare new physicians to serve patients of all ages with compassion and excellence. This effort is a vital step in improving access to healthcare, reducing disparities, and ensuring that families in our region have consistent, high-quality care for generations to come.
This grant allows the organization to grow the future of healthcare right here in Missouri. We are grateful to the State of Missouri for investing in our community, and we look forward to working with our partners to support the next generation of physicians.
The application deadline for the first class of Family Medicine residents is November 15. The inaugural class will begin training in July 2026.

Dr. Kristi Crymes and Dr. Katie Davenport-Kabonic are facilitating a new lifestyle medicine program offered to adult patients with type 2 diabetes. LEADR (Lifestyle Empowerment Approach for Diabetes Remission) is a 12-week lifestyle medicine intervention delivered via Shared Medical Appointments (SMAs). It’s designed for type 2 diabetes (T2D) REMISSION, using a reimbursable, flexible curriculum. The curriculum has been developed and studied by the ACLM showing very promising outcomes. CoxHealth Family Medicine Residency is part of an ACLM multi-site pilot study.
Multiple physicians from MAFP were involved in the Summer Retreat of the Family Medicine Leadership Consortium in Alexandria, VA, including Upagya Kompalli, MD, and Barbara Miller, MD, from Freeman Health System in Joplin, and Sarah Cole, DO, from Mercy in St. Louis.
The retreat brought together leaders from across the country to discuss the future of family medicine, with sessions focused on redefining foundational elements of care, advancing research capacity, and exploring innovations such as artificial intelligence and point-of-care ultrasound.

DO YOU HAVE NEWS TO SHARE? Email it to office@mo-afp.org for review. We love to hear from our members!
Ishak Hossian, MD, a PGY3 at SSM Saint Louis University Family Medicine Residency Program, has been selected as a recipient of the 2025 American Academy of Family Physicians Award for Excellence in Graduate Medical Education. This prestigious national honor recognizes outstanding family medicine residents who demonstrate exceptional leadership, academic performance, patient care, and community involvement.
Dr. Hossian will be celebrated at the AAFP Family Medicine Experience (FMX) in Anaheim, CA, in October. Congratulations!


Josephine Glaser, MD, FAAFP, was recently presented with the AMA Women Physicians Section (WPS) Inspiration Award. This award honors and acknowledges physicians who have offered their time, wisdom, and support throughout the professional careers of fellow physicians, residents and students. Congratulations, Dr. Glaser!



• Locations include Springfield, Missouri, and surrounding communities
• Top 100 Integrated Health System
• Voted Modern Healthcare Best Places to Work five times Benefits
• Competitive salary
• Comprehensive benefits package
• Sign-on bonus
• Relocation allowance












The Bothwell-University of Missouri Rural Family Medicine Residency trains service-oriented, evidence-based family medicine physicians to provide outstanding care and leadership for rural patients and their communities.
THIRD-YEAR RESIDENTS


FIRST-YEAR RESIDENTS


SECOND-YEAR RESIDENTS




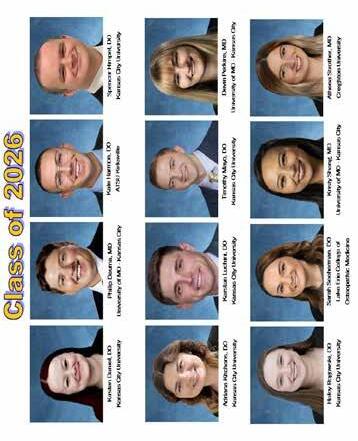

















































































F a m i l y M e d i c i n e 2 0 2 52 0 2 6 R e s i d e n t s M a y w r i t e o r d e r s & p r e s c r i p t i o n s M a y p e r f o r m p r o c e d u r e s M a y p e r f o r m H & P s a n d p a t i e n t v i s i t s




















FRIDAY, NOVEMBER 7, 2025
7:00-8:00 am Registration and Breakfast Buffet with Exhibitors
8:00-8:45 am Missouri in Transition: Aligning Healthcare, Policy, and Public Health
Heidi Miller, MD
MODepartment of Health and Senior Services Chief Medical Officer
8:45-9:30 am Beyond the Trauma: Practical, EvidenceBased Strategies for Diagnosing and Managing PTSD in Family Meidicine
Jay Lee, MD, MPH, FAAFP
9:30-9:45 am Break with Exhibitors
9:45-10:30 am Revisiting Common Dermatologic Conditions: Considerations for Skin of Color
Sofia Chaudhry, MD
10:30-11:15 am Intorduction to Dermoscopy in Primary Care
Lane Wilson, MD, FAAFP
11:15-11:45 am Break with Exhibitors
11:45-12:15 pm Family Medicine Forward: MAFP Annual Meeting Luncheon
12:15-1:15 pm From Clinic to Capitol: Advocacy in Action MAFP/AAFP Update
Peter Koopman, MD, FAAFP & Sarah Cole, DO, FAAFP
MAFPAdvocacy Committee Co-Chairs
Jay Lee, MD, MPH, FAAFP, AAFP Board Member
1:15-1:30 pm Break with Exhibitors
1:30-2:15 pm Navigating Gastrointestinal Challenges: Insight into GERD and H. pylori Management
Jonathon Firnhaber, MD, MAEd, MBA
Annenberg Center for Health Sciences
2:15-3:00 pm BRIDGING COMMUNITY: Collaborative Efforts in Early Detection and Intervention for Alzheimer's Disease
Brianna Wynne, MD Medical Learning Institute
3:00-3:15 pm Break with Exhibitors
BREAKOUTS
3:15-4:45 pm Procedural Injection Workshop - Shots that Count: Mastering Injections in the Office
Charles Orth, DO, FAOAO
3:15-4:00 pm Infectious Complications of Addiction
John Cascone, MD
4:00-4:45 pm A Primary Care Perspective on the Diagnosis and Treatment of Irritable Bowel Syndrome
Brooks D. Cash, MD, FACG, AGAF, FASGE
Academic CME
6:00-9:00 pm MAFP Awards Banquet - Great Medsby Rooftop Ballroom - Dress to Impress in 1920's attire!
SATURDAY, NOVEMBER 8, 2025
7:00-8:00 am Sunrise Walk to Nelson-Atkins Museum of Art
7:00-8:00 am Registration & Breakfast Buffet with Exhibitors
8:00-8:45 am Long COVID: What every Primary Care Provider Should Know about the "B-Side" of the Pandemic! Farrin Manian, MD, MPH, FACP, FIDSA, FSHEA
8:45-9:30 am Refugee Health: Essential Considertations for the Practice Physician
Mihiret Belihu, MD
9:30-10:00 am Break and Prize Drawings with Exhibitors
10:00-10:45 am AI: What is There for Me to Use Now and Tomorrow?
Michael Brown, DO David Voran, MD
10:45-11:30 am Paddles and Pains: A Case-Based Approach to Diagnosing and Managing Common Pickleball Injuries in Primary Care
Kevin Gray, MD, FAAFP, MBA, CAQ-SM
11:30-12:30 pm Lunch
12:30-1:15 pm PrEP Yourself
Kento Sonoda, MD, AAHIVS, FAAFP, FASAM
1:15-2:00 pm Osteoporosis Treatment OptionsWhich to Choose?
Kathryn Diemer, MD
2:00-2:15 pm Afternoon Break
2:15-3:45 pm Osteopathic Approach to Low Back Pain Workshop
Jayme Decker, DO, FAAFP George Chou, DO
3:45-6:00 pm Explore the Plaza
6:00-8:00 pm Dine Around on the Plaza with Colleagues - Choose Your Restaurant at the Conference
SUNDAY, NOVEMBER 9
9:00 am Board Meeting
722 West High Street
Jefferson City, MO 65101
