6
Technology Karen Booth Chief Clinical Adviser (Nursing) for the Australian Digital Health Agency
In Conversation Amy Sarcevic Contributing Writer at Hospital + Healthcare
16
Facility admin Emma Bucholtz Senior Lawyer at LegalVision 10,
Column Dr Kate O’Hara FANZCAP (Neonatol., Paeds), Vice-President of Advanced Pharmacy Australia (AdPha) 26
Facility admin Gerry McCusker Managing Director of The Drill

Technology Mathew Cherian Managing Director of MasterCare

Editor: Dr Joseph Brennan, PhD hh@wfmedia.com.au
Publishing Director/MD: Janice Williams
Art Director/Production Manager: Linda Klobusiak
Art/Production: Marija Tutkovska
Circulation: Alex Dalland circulation@wfmedia.com.au
Copy Control: Ashna Mehta copy@wfmedia.com.au
Advertising Manager: Kerrie Robinson +61 400 886 311 krobinson@wfmedia.com.au
Business Development Manager: Andrew Jackson +61 400 604 646 ajackson@wfmedia.com.au
PUBLISHED BY Westwick-Farrow Media
A.B.N. 22 152 305 336

Key insights await you in this edition. For our lead feature: in the context of the Sharing by Default to My Health Record initiative, the Australian Digital Health Agency’s Chief Clinical Adviser (Nursing), Karen Booth, sets out why it’s time for secure and seamless health data exchange, complete with a supportive case study by emergency physician Dr Xiu Lee.
www.wfmedia.com.au
Head Office Unit 5, 6-8 Byfield Street, North Ryde Locked Bag 2226 North Ryde BC NSW 1670 AUSTRALIA ph: +61 2 9168 2500
If you have any queries regarding our privacy policy please email privacy@wfmedia.com.au
Subscriptions for unregistered readersprice on application
Printed and bound by Ive Group Print Post Approved PP100022780 ISSN 2204-3438 PRINT ISSN 2204-3446

Westwick-Farrow Media is committed to using environmentally responsible print services to produce our publications. This edition is made with a mixture of materials from FSC-certified forests, recycled materials, and/or FSC-controlled wood. While controlled wood doesn't come from FSC-certified forests, it mitigates the risk of the material originating from unacceptable sources . It is delivered in a totally degradable plastic wrapper.
In our regular In Conversation series, we speak with Australia’s new Chief Medical Officer, Professor Michael Kidd AO — just two months into the role, he is already waist-deep in plans to improve the nation’s health. Also in a future-focused leaders space, with the effects of day hospital underfunding being felt across health care, we sit down with Day Hospitals Australia CEO Jane Griffiths to ask “Where to from here?”
In the legal sphere, Emma Bucholtz — Senior Lawyer at LegalVision — covers the new wage theft federal laws that came into force this year, setting out the changes, how compliance can be ensured and best-practice prevention procedures; while for a design reprieve, our Design in Health series has Queensland’s new Bundaberg Hospital in its sights — due for completion in 2027, we soak in the three themes woven into its design: land, geology and water.
Then in another of our regular series, we spend A Day in the Life of Brad Butt, a men’s health pharmacist. In addition to a fresh start
at his Fyshwick Pharmacy in Canberra, Brad takes us through his passion project, Mens Health Downunder. Currently preparing to launch a men’s health urological service in Ireland, Brad’s day marks an evolution for us as well; in a series first, Brad adds another dimension to his day, sharing a video from Dublin amid launch preparations — so have your phone at the ready to scan the QR code on page 21.
Also in this issue, a crisis simulation and training specialist sets out an ‘audit, educate, simulate’ crisis planning ethos in the wake of Healthscope’s fall into administration; AdPha Vice-President Dr Kate O’Hara FANZCAP has a message about pharmacy’s role in a healthier, greener future; we deep dive into some recently published Australian research; plus more, including a spotlight on some interesting case studies across health care.
I hope you enjoy the read.
Dr Joseph Brennan, PhD Editor, H+H hh@wfmedia.com.au

We welcome articles and research reports from health professionals across Australia for review for the bimonthly print publication and our daily web page. If you have a story you think would be of interest, please send an email to hh@wfmedia.com.au











and consumer-centred

The future of digital health is not just approaching the horizon; it is already here. In the context of the Sharing by Default to My Health Record initiative, the Australian Digital Health Agency’s Chief Clinical Adviser (Nursing) sets out why it’s time for secure and seamless health data exchange — and an emergency physician provides a supportive case study.
In health care, accurate and timely information can mean the difference between effective treatment and avoidable complications. It can even be the difference between life and death. As a nursing professional, I have seen firsthand the challenges that arise when vital patient information is inaccessible. Nurses, often the frontline providers of patient care, rely heavily on accurate data to make informed decisions, administer medications safely and monitor patient progress. Yet, for decades, Australia’s healthcare system has relied on outdated information-sharing models, where consumer data is locked in disconnected silos, accessible only to a select few. This approach, once acceptable in an era of filing cabinets and fax machines, no longer serves modern healthcare needs.
I view the transition of traditional healthcare information like an old-fashioned key and lock system. Imagine consumers having multiple keys, each one granting access to different parts of their health information, stored in separate locked cabinets. If a new healthcare provider joins their care team, they would need to acquire all the specific keys to unlock the needed information. In contrast, modern digital health acts like a personal safe deposit box for the consumer. They hold the master key, giving them the power to control who can access their health data, ensuring it is always within reach for healthcare providers involved in their care.
This centralised repository allows for seamless sharing and retrieval of all pertinent information, making sure no critical detail is overlooked or inaccessible. As consumers’ healthcare needs evolve, they retain control over their data, ensuring timely and secure access for their dynamic care team. Of even greater importance is that consumers use their health information to help inform choices about their own care.
Karen is an influential leader who has been advocating for the role of nurses in digital health for many years. She has been a key contributor to the advancement of digital health in the nursing profession and played a pivotal role in the future of the Australian healthcare system as a member of the Strengthening Medicare Taskforce and has participated in numerous national health policy advisory groups, including providing advice to the Primary Health Care Advisory Group, the MBS review and Primary Health Reform Steering Group for the National Primary Health Care 10 Year Plan.

The future direction of health care is at a crossroads, where technology must evolve to match consumer expectations. Australians now expect their health data to be in their control and available when and where they need it, just as they expect instant access to banking, travel and communication tools. The federal government’s Sharing by Default to My Health Record initiative marks a major turning point in delivering secure, real-time interoperability, ensuring that health information is consumer-controlled, discoverable, accessible and shareable between healthcare providers involved in their care. Legislative changes will ensure key health information, starting with the upload of pathology reports and diagnostic imaging results by default to My Health Record, will empower consumers to take charge of their key health information and allow healthcare providers to access real-time data. This is an opportunity that is as critical as it is exciting.
This crucial sharing of information reminds me of a conversation a colleague once had with an emergency nurse on the importance of having real-time patient data. They described an emergency situation when they spent half an hour calling radiology providers to see if they were “the blue place around the corner from a servo” that a distressed patient described as having a critical scan result. They agreed it was time that could have been better spent with the patient.
For me, the benefits of interoperability in a hospital setting are clear. Consider, for example, an unconscious patient in the emergency room with no one else present to provide their medical history. Healthcare providers on the front line waste precious
The real measure of success won’t be gauged by ‘system uptime’ or ‘authentication compliance’, but by situations like when an emergency nurse can instantly access the right scan at the right time to make a potentially lifesaving decision.
minutes chasing down scattered medical records, hoping to piece together a lifesaving treatment plan. They may be unable to determine whether the patient has allergies, chronic illnesses or medications that could interact dangerously with emergency treatment. With information going into My Health Record by default, this can be retrieved as soon as the patient’s identification is confirmed, allowing healthcare providers to make clinical decisions with more confidence. The time spent hunting for old results will be a thing of the past.
While it’s important to continue supporting processes that help vulnerable and less digitally connected Australians, there are a growing number of people who are increasingly digitally savvy and expect seamless, user-friendly digital health solutions. They want access to their health information to make better choices about their health and care. Undoubtedly, this expectation presents many challenges, as the industry grapples with privacy concerns, cybersecurity risks, and the overarching
responsibility of ensuring that health data remains secure and trusted.
At the Australian Digital Health Agency (the Agency), these challenges are taken seriously and managed through a Conformance Framework which ensures that digital health tools meet rigorous security standards, protecting consumer privacy while enabling seamless data exchange. It outlines the processes through which healthcare organisations and their software vendors can assess and demonstrate their alignment with the national standards. The specifications outlined in the Conformance Framework detail conformance profiles that show how software must behave to ensure data is managed securely, safely, and in line with legislative and policy expectations.
A conformance profile is like a checklist that shows whether a digital health system follows specific technical standards. It helps ensure that different systems can safely and reliably share information with each other by using standard language, rules and behaviours.
While the rules that underpin the Sharing by Default legislation are still being finalised, there is no doubt that existing
conformance processes will be leveraged and strengthened. This will help the sector adapt to the new requirements without compromising the safety and security of consumer information.
As Sharing by Default expands, it is not just higher data volumes that drive the need to update conformance profiles — it is also about ensuring we remain at the forefront of digital health innovation. When profiles are updated, it’s vital to guide the sector through the changes, including setting an expiry, or sunset date, on older conformance profiles. The Agency collaborates closely with developers to ensure systems are up to date.
Shaping the future of digital health for all Australians
Digital health is not solely about efficiency; it’s also about equity. A truly connected healthcare system ensures every Australian, regardless of location or circumstance, has access to the same high-quality care. As the capabilities of My Health Record expand, the Agency is co-designing these solutions with consumers, healthcare providers, software vendors and policymakers, because a modern healthcare system is only effective if it is trusted, accessible and built for the people it serves.
As digital health leaders, we must do more. Our role is to ensure the sector is not only prepared for the coming change but actively shaping it. We must align incentives, enforce conformance and, most importantly, protect the trust Australians place in our health system. The real measure of success won’t be gauged by ‘system uptime’ or ‘authentication compliance’, but by situations like when an emergency nurse can instantly access the right scan at the right time to make a potentially lifesaving decision. That is what digital health can and must deliver. That is the promise of Sharing by Default, founded on conformance requirements that make information-sharing secure, valuable and dependable for all Australians.
The future of digital health is not just approaching the horizon; it is already here. It’s time to remove the silos that prevent connected care. It is our responsibility to ensure that every consumer, provider and policymaker is ready for it.
This shift towards more digitally enabled models of care also highlights the importance of a skilled, adaptable workforce. Attracting and developing digital capability across health professions is critical to sustaining innovation and ensuring long-term system resilience. The Agency works with universities, research institutions and professional bodies to embed digital health competencies into medical, nursing and allied health education. By modernising training and showcasing the role of digital tools in improving care, we can help make health professions more appealing to the next generation and strengthen Australia’s position in digital health leadership.
*Karen Booth is the Chief Clinical Adviser (Nursing) for the Australian Digital Health Agency and immediate past president of the Australian Primary Health Care Nurses Association (APNA).
BY DR XIU LEE*
The frequent challenge in Emergency Medicine is seeking out relevant patient information in a fragmented healthcare system short on time and resources.
Sometimes, you need the detective skills of Sherlock Holmes to solve the mystery of where and when the patient had their last investigations done. Hunting down these records can often involve phoning multiple providers in the search for clues to the missing data.
Trying to hunt down patients’ results sometimes involves working out where they even had the investigations done and phoning multiple possible providers. This wastes time that would be better spent providing actual clinical care to the patient, or to the many other patients still waiting to be seen. Unfortunately, this is not a task we can delegate to administration staff.
More difficulties arise because people often present to the ED outside of typical business hours, when they are unable to access their usual healthcare providers. This means that the GP clinics they attend are not available for us to contact for health summaries or important investigation results. Many private radiology providers also have no after-hours options for us to get results.
If doctors send patients to hospital because of abnormal pathology results, we will often repeat pathology in the ED to exclude a false result before starting treatment.
However, we still need to know what the abnormal result was. There have been many occasions where the patient does not even know what result was abnormal. They simply say that their doctor phoned and told them to go to Emergency.
We usually also need to know what a patient’s previous pathology results were to have a baseline comparison. If a patient has impaired renal function on blood tests
in Emergency, our approach differs if this is new for them, as opposed to if it is normal for them due to a chronic condition. It can mean needing a host of extra tests and hospital admission or alternatively being able to discharge someone.
Sometimes, patients present with ongoing symptoms that have already been recently investigated by their usual healthcare providers. Take, for example, a patient with abdominal pain who has had a CT just a few days ago for the same symptoms. Attempts would usually be made to try to obtain that result rather than repeat the CT, to avoid exposing the patient to unnecessary radiation. What that has sometimes meant, when the radiology provider was uncontactable for the result, was that we had to keep the patients in Emergency overnight until the provider was available in “business hours”. This has flow-on impacts for ED capacity, affecting available space to see other patients.
To avoid errors, it is vital to have a copy of the result, rather than just a report over the phone. However, there is often a delay in having results sent through (usually faxed, less commonly emailed) after we have managed to contact the external investigation providers. This can mean multiple subsequent follow-up phone calls to chase up results that have not arrived as expected.
Having near real-time access to patient investigation results would provide us with a faster and more accurate picture of the patient’s condition so we can determine next steps. This means patients would avoid having to wait extra hours in Emergency for us to get results, which has benefits for not only the individual patient, but the efficiency of the entire system. It will mean physicians such as myself can go back to doing what we do best, providing emergency health care, and we can leave the detective work to the likes of Sherlock Holmes.
*Dr Xiu Lee is an Emergency Physician and Digital Health Adviser based in Melbourne. She brings with her a practical eye for how health technology needs to fit into the realities of a fast-paced clinical environment, where essential information must be quickly available 24/7.

AMY SARCEVIC*
The effects of day hospital underfunding are being felt across health care. To understand current challenges and chart a sustainable path forward, Hospital + Healthcare speaks with Jane Griffiths, CEO of peak body Day Hospitals Australia.

Day procedures, like colonoscopies, are commonly performed in traditional ‘overnight’ hospitals, but moving them into day hospitals could save the healthcare sector millions, according to an analysis by Day Hospitals Australia.
The analysis reveals how flaws in the current healthcare funding model overcompensate traditional hospitals for day procedures; at the same time, under-incentivising day hospitals who can do them more cost-effectively.
The data
In the realm of gastroenterology, overnight hospitals are paid 93% more than day hospitals, yet account for 73% of procedures. Moving diagnostics alone into day hospitals would save insurers $182 million annually, says Day Hospitals Australia CEO Jane Griffiths.
“Essentially this data shows us that the day hospital sector is probably underpaid a little, but that the overnight sector is paid far too much for these procedures,” she said.
“And this is just one example. Now try and comprehend the financial impact across the full breadth of gastroenterology procedures — not just diagnostics — and other specialities, too.
“It’s an eye-watering amount of unnecessary expenditure; even so, the same-day trend prevents overnight hospitals from crosssubsidising other, more complex procedures.”
Indeed, the report showed equally concerning findings in the realm of chemotherapy, where the indexation for day hospitals has risen
11% since 2014, compared with 32% for the overnight sector. If all chemotherapy were to be carried out in day hospitals, the sector would save $35.7 million annually.
Across the top 20 diagnostic-related groups, the same shift would save $0.5 billion dollars.
At the heart of this issue, Griffiths says there are misconceptions on what a day procedure is, which stops funding from being channelled appropriately.
“A procedure is classed as day stay if it can be done in less than 24 hours,” she said. “But we are seeing confusion around this across the public and private sector.
“Some falsely assume that if a patient is admitted at 9 am and discharged at 1 am, it is as an overnight stay.
“A procedure of this length is always day stay, according to the international definition, and hence is appropriate for care in a day hospital,” she clarified.
Even with an agreed definition, Griffiths highlights that day hospitals tend to have weak bargaining power in their negotiations with insurers.
She says large corporate hospitals are in the front seat, with “most of the pool going to them” and day hospitals “picking up the pieces”.
Not helping matters, day hospitals are underrepresented on government forums and often go unheard in policy discussion, she said.
“The CEO Forum that the Minister [the Hon Mark Butler MP] set up, after his private hospital financial health check last year, doesn’t have any peak bodies, like mine, on it,” Griffiths said.
“It has actual CEOs from hospitals; but unfortunately, only one day hospital representative on it. And that representative is great. But he comes from a large corporate day hospital group.”
The result is lack of incentives, with existing funding mechanisms often failing to cover basic costs for procedures like colonoscopies.
“Reimbursement doesn’t cover the cost of running the day hospital. So, when you see the overnights being paid so much more, it’s soul-destroying,” Griffiths said.
With private facilities still hurting from COVID, existing funding constraints mean an uncertain future for day hospitals.
“If it wasn’t for [former] Minister Hunt’s viability agreement, a lot of hospitals — large and small — would have disappeared. We’ve already lost 23 day hospitals in the last two years — and 11 of those have been gastro units, which is alarming,” she said.
What’s
Griffiths says shifting all day procedures into the day hospital sector at once would harm overnight hospitals, but that a gradual shift — like the US experience — could work.
“The US did exactly that. They transferred ophthalmology and gastro first and then just

Funding aside, Griffiths says day hospitals are often a preferred choice for patients.
“Patients in day hospitals are happy with their experience. They like the hospital size, with a nonthreatening environment, easy access and limited time required in hospital.
“Their procedures have been refined to such a degree that they can be discharged home relatively quickly after their procedures.”

gradually started introducing other specialties into the ambulatory surgery centres.”
To facilitate the shift, she recommends the introduction of a ‘Type D’ category that would mean a same-day procedure must be done in a standalone day hospital.
This would add to the current classification system, in which Type A requires treatment in an overnight hospital, Type B is day case venue not stipulated and Type C is treated out of hospital unless certified for hospital treatments.
Given the benefits, she said this would represent a win for patients and the private hospital sector.
“It would generate significant savings and free up funds for complex procedures in overnight hospitals,” she concluded.
*Amy Sarcevic is a freelance science and technical writer who regularly writes for Hospital + Healthcare. She has an academic background in psychology.










Boasting a modern design that is approachable and intuitive, the currently-in-progress new Bundaberg Hospital is set against a backdrop of subtropical bushland. Shielded from major roads by landscaped spaces, the building offers a welcoming environment where staff, patients and visitors can enjoy the outdoors, with a design intended to make it blend seamlessly into its surroundings. This creates a strong civic presence that’s easily recognisable upon approach.
The building is being delivered by COX and lead architect BLP, working as part of the CPB Contractors consortium, along with Queensland Health (Health Infrastructure Queensland) and Wide Bay Hospital and Health Service. COX was responsible for the exterior, façade and structure, describing the architecture as one that reflects a commitment to cohesion, with every element — from the façade to the interiors and landscape — coming together for a unified, visually striking experience.
Three key themes were used as inspiration and woven into the design: these were land, geology and water, to form the hospital’s character and connection to the region. For land, the region’s status as a rich fruit bowl served as inspiration, with volcanic soils and the presence of remnant bushlands and diverse flora and fauna; for geology, Bundaberg’s coastline erosion, highly productive agricultural soil, sandy beaches and enduring volcanic basalt rock was drawn on; and for water, the Burnett River, creeks, dams, floodplains, streams and watercourses within the Bundaberg area, and the southern tip of the Great Barrier Reef, influenced the design. >

Three key themes were used as inspiration and woven into the design: these were land, geology and water, to form the hospital’s character and connection to the region.
The $1.2 billion new Bundaberg Hospital will include: 320 overnight beds, with more single rooms for patient comfort and privacy; a larger ED and range of outpatient and diagnostic services; more operating theatres and recovery spaces; acute services, including medical, intensive care, surgical, maternity, mental health, paediatric care and renal services; clinical support spaces for medical imaging, pharmacy, sterile services, outpatients, mortuary and pathology; teaching, training and research spaces; and a rooftop helipad on the main acute building.
With an architectural concept that aims to push the boundaries of a traditional healthcare facility, this new hospital aspires to be a living, breathing testament to the identity and spirit of Bundaberg, where architecture, culture and community converge to create a healing environment deeply rooted in its surroundings. It is due for completion in late 2027.


In healthcare and aged care, cleaning and hygiene are more than routine — they’re essential to safety and care quality. With increasing expectations around infection control, sustainability, and operational efficiency, staying ahead of the curve is critical.
This 29–30 October, healthcare, aged care, and facility professionals will gather at the ISSA Cleaning & Hygiene Expo 2025, held at ICC Sydney — Australasia’s leading event dedicated to cleaning and facility management solutions.
Featuring 70+ exhibitors, the Expo will spotlight cutting-edge solutions tailored for the healthcare and aged care sectors — from autonomous robots to sustainable cleaning agents and infection-control technologies.

Attendees can connect directly with suppliers, compare innovations, and gather insights to inform purchasing and operational decisions in complex care environments.
Over two days, the Expo’s education program delivers practical, expert-driven insights across core industry challenges. Must-attend sessions include:
• Invisible Risks, Visible Impact: Tackling HAIs Through Professional Cleaning
This panel addresses the persistent threat of Healthcare-Associated Infections (HAIs), presenting Australian and global data on high-risk zones and evidence-based cleaning strategies. Attendees will walk away with actionable insights on how to reduce HAIs through professional cleaning, targeted training, and strict compliance.
• Robots & Care: The Future of AI and Automation in Cleaning
As facilities face labour shortages and higher compliance standards, robotics and AI offer real solutions. This session explores how automation is being deployed in hospitals and care settings across Australia and internationally — offering perspectives

on implementation, ethics, and measurable outcomes for efficiency and safety.
Innovation will be on display in the ISSA Innovation Zone, where visitors can explore shortlisted products from the ISSA Excellence Awards. Categories include everything from cleaning agents to sustainable solutions, with winners announced live on the show floor.
The People’s Choice Award, voted on by attendees, adds an engaging layer of participation, highlighting the solutions that resonate most with frontline professionals.
Another highlight will be the ISSA Emerging Leaders Awards, recognising rising stars under 40 who are driving change across the cleaning and hygiene sector — including in healthcare and aged care environments.
The Expo isn’t just about products — it’s about people. A networking function on 29 October, brings together suppliers, buyers, and healthcare professionals for a relaxed opportunity to connect, exchange ideas, and celebrate Excellence Award winners.
For professionals working in infection prevention, procurement, environmental services, and facility operations, these

connections can lead to future partnerships and innovative solutions.
The ISSA Cleaning & Hygiene Expo 2025 offers:
• Exposure to the latest cleaning technologies and best practices
• Practical education on infection prevention and operational resilience
• Firsthand experience with robotics, AI, and other high-tech solutions
• A chance to benchmark against industry leaders
• A platform to grow your network and collaborate on future-ready strategies
Whether you manage facility services, oversee infection control, or source equipment and supplies, this event delivers tools and knowledge to support better care outcomes.
Join us 29–30 October at ICC Sydney and discover what’s next in healthcare and aged care cleaning.
Register now at: cleaninghygieneexpo.issa.com
EMMA BUCHOLTZ*

From 1 January 2025, an employer that intentionally underpays wages or entitlements owed to an employee may be committing a criminal offence.
The Fair Work Ombudsman can now investigate suspected underpayment offences and refer matters for prosecution.
Businesses and individuals can also face significant monetary penalties.
To avoid unintentional underpayments, employers should implement robust payroll systems, conduct regular audits, seek legal advice and maintain accurate records of employee entitlements.
New wage theft federal laws came into force this year. A lawyer sets out the changes, how compliance can be ensured and best practice prevention procedures.
Wage theft is becoming increasingly prevalent in Australia. To address this issue, the Australian Government has introduced new laws. It is essential that healthcare providers understand their legal obligations, as failure to do so can result in criminal charges and penalties.
This article will cover the meaning of wage theft, changes to the law criminalising wage theft across Australia, enforcement and penalties for non-compliance, and best practice for avoiding underpayments in the healthcare sector.
The term ‘wage theft’ refers to employers underpaying their employees, therefore stealing from them. Wage theft, however, is not always malicious and can happen by mistake. In this sense, wage theft can take two forms: deliberate theft and accidental theft. Australian law now clearly distinguishes between deliberate and accidental wage theft, with the former amounting to a criminal offence and attracting significant penalties.
The Closing Loopholes amendments to the Fair Work Act 2009 (Cth) made it a criminal offence to intentionally underpay employees’ wages and certain entitlements. Under the
new laws, which commenced on 1 January 2025, a healthcare employer may commit a criminal offence where:
• an amount was owed to an employee under the Fair Work Act, a modern award, enterprise agreement or other relevant legislation (eg, wages, allowances, paid leave or superannuation); and
• the employer intentionally failed to pay, or neglected to pay, the amounts when they were due.
An employer can be a company or an individual. Third parties who participate in or assist with violating wage theft laws can also face criminal prosecution.
Honest mistakes and unintentional miscalculations will not amount to a criminal offence under the new laws. However, healthcare employers must be able to prove that their conduct was not intentional.
The Fair Work Ombudsman (FWO) has powers to investigate alleged wage theft and may refer matters to the Commonwealth Director of Public Prosecutions or the Australian Federal Police for prosecution where there is sufficient evidence of intentional non-compliance.

Healthcare employers prosecuted for wage theft offences may face:
• a maximum of 10 years’ imprisonment; and/or
• a maximum monetary fine, being the greater of:
• three times the underpayment amount (if this can be determined); or
• $1.585 million for an individual and $7.825 million for a company.
While penalties for non-compliance are severe, the new laws also provide a ‘safe haven’ to encourage business owners to come forward and report possible wage theft. One option allows business owners (or individuals responsible for wage theft) to work with the FWO through a cooperation agreement. Small businesses with fewer than 15 employees may avoid prosecution if they can show they are following the new Small Business Wage Compliance Code.
Even with the new laws in place, the FWO can still issue compliance notices, orders or take civil action if businesses do not comply.
An experienced employment lawyer can help determine the best course of action if you believe you, or anyone else in your healthcare business, has engaged in wage theft (either intentionally or as an honest mistake).
As a healthcare employer, one of your main priorities should be correctly paying your employees their owed wages and entitlements. Before hiring staff, you should carefully consider your minimum pay obligations and ensure you and your business can meet these.
Before hiring a healthcare employee, you should:
• familiarise yourself with the National Employment Standards under the Fair Work Act 2009;
• research and seek advice on whether your employees are covered under a modern award or an enterprise agreement; and
• implement efficient and accurate timekeeping processes and maintain records of time worked and entitlements accrued.
Modern awards set out the standard terms and conditions of employment across various industries and occupations. Many healthcare workers employed by private sector employers are covered by the Health Professionals and Support Services (HPSS) Award on an industry basis.
However, some occupational awards may cover employees who cannot be classified under the HPSS Award (or another industry award), such as the:
• Nurses Award 2020;
• Medical Practitioners Award 2020;
• Ambulance Award 2020; and
• Clerks Award 2020.
Public sector healthcare employees are generally covered by a State reference public sector award.
Each modern award sets out minimum entitlements for various roles within the healthcare sector and contains sophisticated classification systems where employees’ qualifications, experience and responsibilities directly impact pay rates.
To mitigate the risk of engaging in wage theft, it is crucial, as an initial hiring step, to:
• identify which employees are covered by the HPSS Award, or other industry or occupational awards;
• familiarise yourself with the classification levels within the applicable award; and
• ensure compliance with award provisions regarding pay rates, allowances and working conditions.
Also, health care often involves shiftwork and irregular hours, making it crucial to understand and comply with:
• minimum wage rates, including any applicable loadings for shift work, weekends or public holidays;
• overtime provisions; and
• industry-specific allowances, such as oncall and uniform allowances.
To avoid criminal wage theft and severe penalties, you should take proactive steps to prevent and remedy any accidental or mistaken underpayment of your healthcare staff. This will mitigate your risk exposure to penalties, develop a culture of trust and transparency in your healthcare business, and protect your reputation as an employer.
Avoid complacency, as the FWO or an individual employee may take other civil action against you and your healthcare business for underpayments. If you believe you may be underpaying your healthcare staff, facing prosecution or need help paying your employees the correct amount, contact your lawyer and accountant for advice.
To avoid intentional wage theft, we recommend that you:
• ensure that payroll systems and processes are established correctly (including by incorporating the correct modern award so that employee entitlements are correctly paid and accrued);
• obtain legal advice quarterly/annually to ensure you are paying your healthcare employees correctly;
• maintain accurate records of your employees’ qualifications, training and experience in the industry, and review these at the point of promotion or advancement;
• ensure you are paying your employees relevant overtime, allowances and penalty rates in line with any modern award or enterprise agreement that applies to them;
• familiarise yourself with complex on-call provisions requiring different rates for availability versus active work periods and industry-specific allowances;
• conduct regular and systematic audits;
• ensure you keep accurate employee entitlement records; and
• implement salary review initiatives.


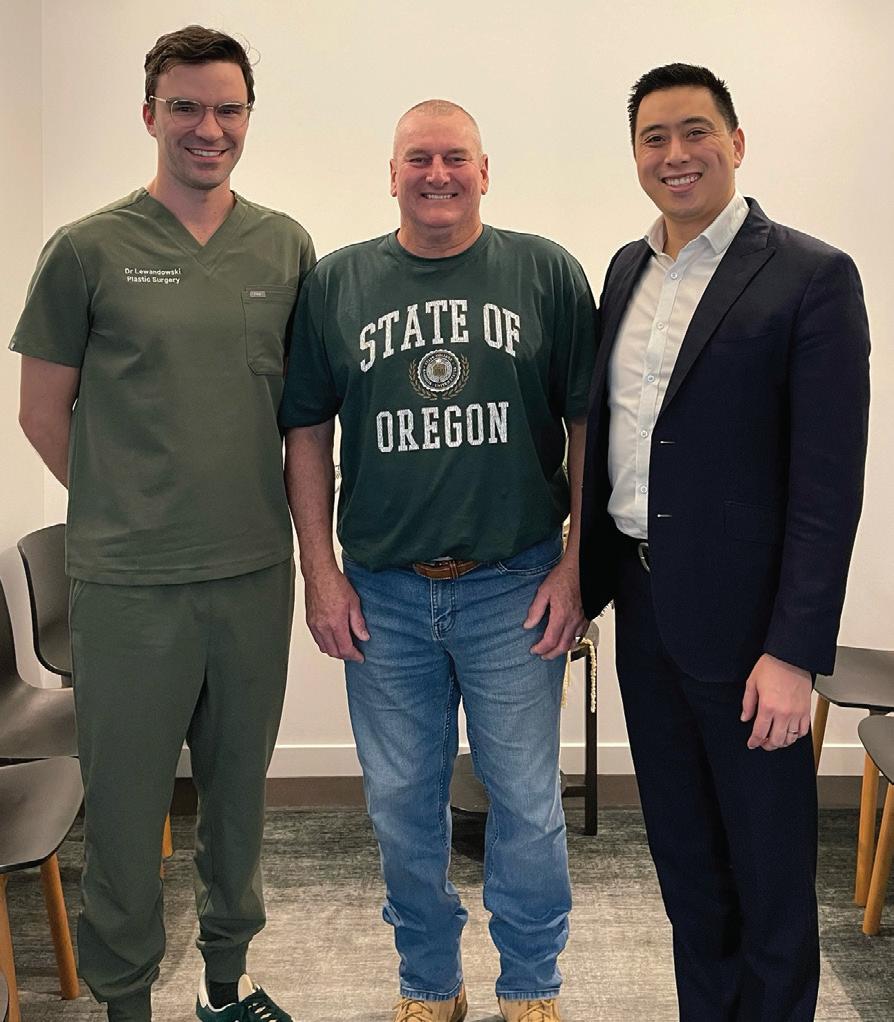
Greenslopes Private Hospital in Brisbane now offers advanced microsurgery for lymphoedema, becoming the state’s first private hospital to do so. Affecting an estimated 70,000 Australians, lymphoedema is commonly seen after cancer surgery involving lymph node removal and can cause chronic swelling, pain, recurrent infections, and significant physical and emotional distress.
Recently completing a lymphaticovenous anastomosis (LVA), which was the state’s first in a private hospital setting, were specialist plastic surgeons Dr Matthew Cheng and Dr Andrew Lewandowski. The case involved a patient with aggressive skin cancer and used intricate supermicrosurgery to help reroute the patient’s lymphatic system and reduce the risk of lifelong swelling and discomfort — a prophylactic LVA being performed during the procedure, connecting tiny lymphatic vessels directly to veins to bypass damaged pathways and help prevent lymphoedema from developing.
“Historically, people with lymphoedema have had very limited options, often relying on compression, massage or simply learning to live with the condition,” Cheng said. “With LVA, we’re offering patients a surgical solution that can ease symptoms or even prevent lymphoedema altogether.”
Lewandowski said the new procedure represents a shift in how hospitals care for people during and beyond cancer treatment. “While we excel at treating cancers and saving lives, we have fallen short on managing the long-term consequences of invasive surgery,” Lewandowski said. “Lymphoedema can impact a person’s ability to perform everyday tasks and put them at greater risk of skin infections such as cellulitis. Being able to prevent or treat this condition is a huge step forward.”

Hospital pharmacy, like all areas of health care, has a responsibility to care for both people and the planet.
Health care has a significant environmental footprint; the Australian health system is responsible for approximately 5.4% of the nation’s total greenhouse gas emissions.1
At AdPha, sustainability isn’t just a goal — it’s embedded in everything we do. It’s one of the five pillars of Yindyamarra 2030, our six-year strategic plan. And earlier this year, we united healthcare voices from across Australia, Europe and North America during our annual MedsAware: Deprescribing Action Week, championing sustainable medicine use led by AdPha’s Grace Wong FANZCAP (MedSafety, MedInfo), founding Member of AdPha’s Climate and Health Specialty Practice Group and founder of Pharmacists for the Environment Australia.
To effectively confront the climate crisis, embedding sustainability into everyday healthcare practice is no longer optional. At a practical level, pharmacists and technicians are already doing this through the responsible disposal of waste and implementation of recycling programs, optimising medication use (including through deprescribing) and educating on greener alternatives (such as asthma inhalers with lower environmental impact), and adopting other eco-friendly practices such as electronic prescribing. In fact, just recently we celebrated Royal Perth Hospital as the first public hospital in Australia to roll out electronic prescribing for inpatients discharging from hospital, cutting paperwork and speeding up care in the process.
As representatives of the pharmacy profession, we believe sustainability must be front and centre, prioritised in prescribing, procurement and all healthcare decision-making.
Through our formal submissions to the Health Technology Assessment (HTA) Review, AdPha called for climate change mitigation and sustainability to be integrated into health care by including greenhouse gas emissions and other environmental impacts in evaluations. Factoring in carbon costs and demanding greater transparency will help drive greener, more responsible choices that benefit both human and planetary health.
Most notably, AdPha proudly represents pharmacy in Monash University’s Transitions to Sustainable Health Systems Consortium, which will soon release a sector-wide guide towards net zero — complete with relevant, practical recommendations for health professionals.
This national consortium brings together leading Australian researchers, healthcare organisations, and government health departments to accelerate emissions reduction, lower healthcare costs and deliver better patient outcomes. Supported by Monash Sustainable Development Institute (MSDI), the initiative focuses on system transitions, emission reduction strategies and behaviour change.
The upcoming guide will recommend actions such as:
• Increasing investment in disease prevention
• Streamlining healthcare services
• Considering environmental impact in procurement
• Minimising clinical and packaging waste
• Switching to renewable electricity
• Phasing out methane gas in health facilities
• Reducing patient travel through virtual care options
AdPha is proud to support the shift towards a more responsible and sustainable hospital pharmacy profession. We look forward to supporting the launch of Accelerating Towards Net Zero: A Guide for the Australian Health System — a vital first step to help health organisations fast-track our collective journey towards a healthier, more sustainable future.
The report is set to be available in October 2025 at www.monash.edu/msdi/transitionsto-sustainable-health-systems-consortium.
1. Australian Government Department of Health and Aged Care. Estimates of Australian health system greenhouse gas emissions 2021–22. April 9, 2025. [Internet] Canberra (AU): Australian Centre for Disease Control;2024. www.health. gov.au/resources/publications/estimates-of-australianhealth-system-greenhouse-gas-emissions-2021-22

Brad Butt completed his studies back in 2007 and since then has been a passionate men’s urological health advocate. Today, Brad splits his time between being that busy ‘chemist’ checking prescriptions and an eclectic assortment of other tasks, and working within his passion project, Mens Health Downunder. While he finds the life and times of a community pharmacist at his Fyshwick Pharmacy vaguely interesting, it’s his involvement with the men of the ACT and, more broadly, his network of like-minded pharmacists in the Mens Health Downunder network across Australia, New Zealand and (soon to launched in) Ireland that sets him apart as truly unique.
05:20 With a super busy work schedule (between the pharmacy and Mens Health) and home life (we have four primary-school-aged kids), finding time for exercise and mindfulness is vital for me. Five days a week it’s a 60-minute run as scheduled by Gavin, my running coach, complemented with two reformer pilates sessions at home in our garage. Canberra really turns it on in winter, so the mornings are not only dark but often subzero. A great time to get some physical activity but also to clear the mind, problem-solve and prepare for the day ahead.
07:30 The pharmacy needs to be opened. Fyshwick is an industrial area and the place is aflush with tradies looking to get a jump on the day ahead; getting supplies, opening their shops, looking for coffee and a brekky roll and, in our case, needing some pharmacy supplies to get through the day. It could be a box of Panadol for the headache, some bandaids for the first-aid kit or a certificate for sick leave. The early-morning requests are mixed and varied and the guys and girls we see early are always great value. We always start the day right.
09:00 The Mens Health Downunder clinic here in Deakin in Canberra opens. Not me today, but it’ll be one of the other Mens Health pharmacists — Tim, Rob or Josh. Patients are booked in like they would be with the GP and we spend around an hour with each patient addressing their needs. This could relate to their prostate cancer recovery, urinary incontinence or erectile dysfunction. Much of what we do is about helping the patient get the best medication, understand how to use it, and get the right medical device (we do a lot of penis pumps, penile clamps and traction devices). All of this takes a lot of time to do well and it’s critical our patients understand what they need to do and what the plan and road ahead looks like.
10:30 Our pharmacy courier arrives and collects the deliveries we have for the morning. These are then delivered to patients primarily at their workplaces. It’s a handy service because everyone is so busy, getting to the pharmacy to put a script in, getting some other items and returning to work can at times be too hard and often adds to the mental load — getting a delivery during business hours really simplifies life for many working folk.
11:00 The vaccinations are now coming in thick and fast. Currently it’s cold, flu, COVID and RSV season, so there is lots of this to do. It’s great to be able to offer this service, and again, I think it’s really convenient for our patients to be able to get a quick and efficient service. Sometimes we will do the vaccinations within the workplace, which is also great as it means staff within these businesses are not inconvenienced in having to get it done outside hours, but also it means they’re vaccinated and are therefore less likely to be taking sick leave as a result of contracting the flu, COVID, etc. Everyone wins.

12:00 The dreaded lunchtime rush! It’s all hands on deck as everyone is coming in to get their medications but also to speak to the pharmacist about their minor ailments. These days, pharmacists are well educated and positioned to help with a range of minor ailments, from urinary tract infections and leave certificates to wound dressings and checking blood pressure or cholesterol.

15:00 Quick presentation to the staff at a local building site on the importance of erectile health and what it can indicate, hence why it’s important to talk about it sooner rather than later. These sorts of chats are always well received, even if some of the participants are not quite sure what they’ll learn before we kick off. Interestingly, I think everyone takes something away from these chats and, not surprisingly, these chats are often the beginning of a meaningful chat with the GP. Life-changing stuff.
13:30 We often have patients seeing their urologists who are referred straight to us. This could be at our Deakin clinic or even at the pharmacy. These patients are always great to see as they help us fill the day and are often needing things pretty quickly. Being able to work alongside their urologists to improve their health and wellbeing is a true honour and something we take a real pride and responsibility in.
19:00 Bedtime — reading books, reflecting on the day and saying goodnight.
16:00 Off to the Mens Health clinic to see how the day was; chase up doctors, book in patients and check messages that need followup. We also review the web orders and see if any of the other Mens Health pharmacists need anything from the head office.
A Day in the Life is a regular column opening the door into the life of a person working in their field of health care. If you would like to share a day in your working life, please write to: hh@wfmedia.com.au

Despite infection controls and sterilisation, bacteria is often found on implants following surgery, which can lead to infections requiring antibiotics. And with antibiotic resistance becoming more common, new preventative measures are needed. Now, an Australian team of researchers — led by RMIT University — have achieved the first reported use of antibacterial coatings made from resilin-mimetic proteins to fully block bacteria from attaching to a surface. It marks a critical step towards the creation of ‘smart surfaces’ that can stop dangerous bacteria — antibiotic-resistant ones like MRSA especially — from growing on medical implants.
“This work shows how these coatings can be adjusted to effectively fight bacteria — not just in the short term, but possibly over a long period,” the study’s lead author Professor Namita Roy Choudhury from RMIT said. “Antibiotic resistance has prompted greater interest in the area of selfsterilising materials and easy preparation of antibacterial surfaces,” Choudhury added. “Therefore, we designed this surface to completely prevent the initial attachment of the bacteria and biofilm formation to decrease the infection rates.”
Applications of such a surface include spray coatings for surgical tools, medical implants, catheters and wound dressings. The protein at the centre of this study — resilin — is known for its elasticity, which allows fleas to leap more than one hundred times their own height in microseconds, and is also known as a biocompatible and resilient protein. "These exceptional properties and non-toxic nature make resilin and resilinmimetic proteins ideal for many applications
requiring flexible, durable materials and coatings,” Choudhury said.
Several forms of coating were created from altered forms of resilin, which were then tested through interaction with E.coli bacteria and human skin cells in lab conditions. What was revealed is that the altered proteins — in nano droplet form, known as coacervates — were 100% effective at repelling the bacteria, while still integrating well with healthy human cells, as is a critical part of medical implant success.
“Once they come in contact, the coating interacts with the negatively charged bacterial cell membranes through electrostatic forces, disrupting their integrity, leading to leakage of cellular contents and eventual cell death,”
RMIT’s Dr Nisal Wanasingha said.
The study — titled ‘Nano-structured antibiofilm coatings based on recombinant resilin’ — was published this year in Advances in Colloid and Interface Science (doi.org/10.1016/j.cis.2025.103530). As to next steps, RMIT’s Professor Naba Dutta said: "These early results are very promising as a new way to help improve infection control in hospitals and other medical settings, but now more testing is needed to see how these coatings work against a wider range of harmful bacteria.” Dutta adding: “Future work includes attaching antimicrobial peptide segments during recombinant synthesis of resilin-mimics and incorporating additional antimicrobial agents to broaden the spectrum of activity.”


Among the challenges faced by kitchen managers in hospitals and other healthcare settings is maintaining exceptional hygiene standards while working within tight budget limitations.
Central to this — with the wellbeing of vulnerable patients to consider — is ensuring that on-site cleaning equipment is capable of achieving the highest level of performance and safety.
This begins with surface cleaning, where chemical dispensers used for dosing concentrated and pre-mixed solutions into sinks, spray bottles and mop buckets must combine precision and consistency with robustness and longevity.
In fast-paced kitchens where excessive force and accidental impacts are common, a robust dispenser casing helps to ensure consistent, reliable performance while reducing the cost of maintenance, repair and replacement.
For the handling of concentrated chemicals, integrated storage enables operators to save space and make cleaning stations tidier and more presentable. This also provides vital health and safety benefits by keeping detergents off the floor and avoiding possible spillage and trip hazards.
Such systems typically feature a cabinetstyle enclosure where various-sized chemical containers can be stored and connected to the built-in dispenser. Lockable cabinets help to prevent theft and tampering and protect employees against exposure to harsh concentrated chemicals.
When it comes to a hospital kitchen’s dishwasher, without an appropriate automatic detergent dosing system the equipment can
be a source of excessive consumption and wastage of chemicals, water and energy.
Therefore, to ensure that crockery and cutlery are washed to the same high standard every time, it’s advisable to install trusted automatic chemical dosing systems that achieve accurate, consistent chemical dosing over the long term.
As the Internet of Things continues to grow, many operators are turning to smart technology to enhance their dosing devices. The inclusion of IoT technology in such equipment can help operators track chemical consumption at their leisure via smartphone, helping them to identify wastage and adjust programming remotely for immediate efficiency improvements.
The incorrect disposal of fats, oils and grease (FOG) in hospital kitchens is a constant challenge for managers, with the build-up of these substances causing drains to block, back up and overflow. This presents a difficult hygiene and odour problem and, despite the best efforts of staff and management to alleviate the issue, the reality is that in such fast-paced environments it is inevitable that FOG will find their way into drains.
A popular solution to this problem comes in the form of drain dosing systems, which periodically dispense an enzyme solution directly into the drain line. This means fats are broken down before they can build up and cause wastewater pipes and drainage systems to block, overflow or release unpleasant smells.
No matter the equipment, the best chemical-handling systems are built using premium-grade components that offer

superior compatibility with even the harshest concentrated solutions.
This means parts are more resistant to degradation from harsh concentrated detergents, helping to deliver repeatable results and extensive equipment lifespan while reducing maintenance requirement.
When it comes to maintaining exceptional cleaning and hygiene standards, it’s clear that a little investment can go a long way. Chemical systems expert SEKO knows this better than most as the company has been helping operators for decades with a dedicated range of dilution, dispensing and dosing equipment.
These include the modular ProMax dilution unit, which dispenses premixed cleaning products into spray bottles, mop buckets and scrubber-dryers, and compatible systems such as the SekureMax chemical storage cabinet. There’s also the IoT-enabled WareDose family of products for use with commercial dishwashers, while SEKO’s DrainDose unit offers a cost-effective, fit-andforget solution to blocked drains lines.

Arecent trial of an interactive game that has shown promise as a treatment for nerve pain could offer hope for a new generation of drug-free treatments. The ‘PainWaive’ technology, developed by UNSW Sydney researchers, offers a potential inhome, non-invasive alternative to opioids — teaching users how to regulate abnormal brain activity linked to chronic nerve pain. UNSW Sydney NeuroRecovery Research Hub researchers Professor Sylvia Gustin and Dr Negin Hesam-Shariati led the recent trial, which, they say, delivered promising results.
In the PainWaive study, which builds on Gustin’s research into changes in the brain’s thalamus (a central relay hub in the brain) associated with nerve (neuropathic) pain,
hundreds of measures across participants’ pain and related issues like pain interference before, during and after four weeks of interactive game play were compared. Participants’ brain activity was tracked via electroencephalogram (EEG) headsets — with the game app responding in real time to shifts in brainwave patterns.
“The brainwaves of people with neuropathic pain show a distinct pattern: more slow theta waves, fewer alpha waves, and more fast, high beta waves,” Gustin explained. “We believe these changes interfere with how the thalamus talks to other parts of the brain, especially the sensory motor cortex, which registers pain.
“I wondered, can we develop a treatment that directly targets and normalises these abnormal waves?” PainWaive was developed in response to this challenge.
For the initial trial, four participants took part, receiving a kit with a headset and a tablet preloaded with the game app, which includes directions for its use. Tips for different mental strategies — like relaxing or focusing on happy memories, to help bring their brain activity into a more ‘normal’ state — were also given, with user data uploaded to the research team for remote monitoring. “After just a couple of Zoom sessions, participants were able to run the treatment entirely on their own,” Hesam-Shariati said.
“Participants felt empowered to manage their pain in their own environment,” HesamShariati added. “That’s a huge part of what makes this special.”
It was found that significant reductions in pain, particularly nearing the end of the treatment, was shown in three out of the four participants and that, overall, the pain relief achieved by the three was comparable to or greater than that offered by opioids.
“Restrictions in the study’s size, design and duration limit our ability to generalise the findings or rule out placebo effects,” HesamShariati noted. “But the results we’ve seen are exciting and give us confidence to move to the next stage and our larger trial.”
Hesam-Shariati also explained that the team had initially planned to use existing commercial EEG systems; however, these either didn’t meet the quality needed to deliver the project or were too expensive — so they developed their own. “Everything except the open-source EEG board was built inhouse,” Hesam-Shariati said. “And soon, even that will be replaced by a custom-designed board.”
Via 3D printing, the team has been able to cut the cost of each headset to around $300 — a fraction of the $1000 to $20,000 price tags of existing systems, Gustin said.
“We’ve worked closely with patients to ensure the headset is lightweight, comfortable and user-friendly,” Gustin said, with the headset using a saline-based wet electrode system to improve signal quality and target the sensorimotor cortex. “Owning the technology offers us the potential to one day offer PainWaive as a truly affordable, accessible solution for at-home pain management, especially for those with limited access to traditional treatments.”
Results of the trial were published this year in The Journal of Pain (doi.org/10.1016/j. jpain.2025.105394). Two further trials are on the horizon. The first, ‘Spinal Pain Trial’, will investigate its potential to reduce chronic spinal pain, while the second, ‘StoPain Trial’, will explore its use in treating chronic neuropathic pain in people with a spinal cord injury.

Total Image Group (TIG) — an Australian uniform and branding provider — teamed up with medical logistics provider Smartways for a customdesigned project. Combining safety standards with brand alignment, the result is believed to be Australia’s first ever red high-visibility garments. Smartways turned to TIG to comply with union-run site requirements of high-visibility uniforms, seeking a solution that could integrate its corporate colours of red and navy into the design, without compromising on compliance with stringent hi-vis standards.
TIG spent 12 months finding the suitable shade of red that would pass safety tests and stay vibrant; something achieved by dyeing the fabric rather than sublimating it, which lends the garments greater
The BOGE EO series scroll compressors are designed to provide completely oil-free compressed air with low vibration and quiet operation. These features make them suitable for sensitive work environments such as dental surgeries, laboratories and hospitals.
The BOGE EO30 Scroll Compressor is the latest in the EO series. With an output of 30 kW, its features include reduced procurement costs and increased efficiency due to changes in performance and dimensions. The EO series now includes models E07, E015, E023 and EO30, all designed to be more compact and efficient.
durability and longevity. Additionally, TIG aided in the Smartways rollout by introducing a new online platform and providing personalised packaging for each employee, ensuring an efficient and smooth transition.
“We couldn’t be happier with the results of this collaboration,” Smartways Marketing Director Steve Cheetham said. “The team at Total Image Group worked closely with us every step of the way, ensuring our vision was brought to life. The red hi-vis uniforms have been a huge success with our staff, who appreciate both the comfort and practicality. Not only do they meet safety standards, but they also perfectly represent our brand identity.”
Total Image Group
www.totalimagegroup.com.au

Key features of the series are completely oil-free compression — to prevent contamination, crucial for sterile environments; a design that minimises noise, making it suitable for close proximity to workstations; low vibration operation that reduces disturbances in sensitive settings; modular design for flexibility and ease of integration; a compact design that requires less space; focus control 2.0, to allow precise adjustment and high-level interface communication with building management systems (BMS); and low maintenance requirements, for long-term reliability and efficiency.
Certain models are available as double systems with a compressed air receiver and either an integrated or external refrigerant dryer. The two-stage cooling concept, featuring a surface cooler and high-quality aluminium aftercooler, promotes optimal output temperatures. Boge Compressors (Australia) Pty Ltd www.boge.net.au
GERRY McCUSKER*
Not all healthcare crises feature rows of banked ambulances, chaotic emergency rooms or equipment shortages. Many, such as Healthscope’s recent fall, take place in the corridors of corporate power or in big boardrooms where risks and threats remain private and hidden — until they become embarrassingly public. In the aftermath of Healthscope’s collapse into administration, a crisis simulation and training specialist sets out an ‘audit, educate, simulate’ crisis planning ethos.
Healthscope’s fall offers salutary lessons about the risks swirling around this vital sector, including increases in chronic diseases, spiralling costs, and problems relating to materials sourcing, remuneration and skills availability. There are pressing concerns for the country’s B2B healthcare supply chain, where many vulnerabilities lurk. The interdependent ecosystem of B2B health care — from pharmaceutical products to device suppliers and essential IT infrastructure — is a virtual Jenga tower. When one block is removed, the knock-on effects can be devastating.
This systemic interdependence means every healthcare organisation needs to reconsider and refresh its crisis-prevention plans — from the risk matrix to its business continuity plans — as well as its issue and incident response strategies. It’s not enough for any healthcare brand to insist its product or service alone couldn’t cause damage, and fail to do any issues or crisis mitigation work. When any item is a critical cog in a larger wheel, there’s scope for both liability or litigation should that item not be available — or perform — when it’s needed most.
Healthcare enterprises must develop, rehearse and learn those plans, processes, roles and responsibilities, which their staff
need to effectively triage, respond to and overcome any presenting risks. So how might a healthcare entity go about getting risk and crisis ready?
The PPRR model: a blueprint for crisis preparation
A durable and usable framework for issues management is the PPRR model: Prevention, Preparedness, Response and Recovery. Think of it as a strategic blueprint for survival; a cyclical ethos asserting that issues and risk management isn’t a one-off event, but a continuous process that helps to mitigate crises.
Prevention is about spotting trouble before it starts. It’s about scanning your environment for possible threats; whether it’s a single point of failure in your own premises or supply chain, or a vulnerability within the wider industry. It might even be changes within your contractual or financial structures.
Preparedness is about making sure you’re ready for the worst; formulating plans and training teams with realistic threat scenarios and building robust contingencies.

Response refers to the sound decisions and appropriate actions that will mitigate damage and protect stakeholder impact. Responses, generally, should be selfless rather than selfish.
Recovery mode is when executives and entities can reflect on how to rebuild with even more resilience than before. What were the key learnings? What were the chinks in our armour? How can we help or best support our people and processes?
The crisis diagnostic: identifying weak spots
An organisation-wide Crisis Diagnostic (aka, a crisis audit) benchmarks your plans and your people against established practice standards.

External experts can bring an independent and dispassionate review of flaws or shortcomings that you may have become blind to. Some simulation providers now offer templated questionnaires that allow companies to checklist their capabilities — and instantly compare them to mandated practices for effective risk mitigation or crisis response.
Crisis simulations: learning by doing A good plan isn’t that good if it’s not known, tried or tested. Obviously, you don’t want to wait for a real disaster to emerge to metaphorically hold your plans and people to the fire; a realistic crisis simulation can recreate the pressures to be faced when a crisis incident occurs.
How would your team react? Would sound decisions be made? Could communication
messages be crafted quickly? Crisis simulators replicate the real-time decisionmaking challenges that will occur. And when employees learn by doing — by interactive learning — core learnings they need are better retained.
The Australian healthcare sector is no stranger to crises; from cyber hacks to employee abuse on social media, to chronic underfunding to suspicious overbilling. Clearly, your organisation cannot leave crisis or risk management to chance. The time to audit, educate and simulate for crises is not ‘another day’ — it’s right now. As the Healthscope furore demonstrates, the community, your customers and your peers demand it.

Australia’s Chief Medical Officer, Professor Michael Kidd AO, has been in his role for just two months and is already waist-deep in plans to improve the nation’s health. Hospital + Healthcare speaks with him to learn more.

The task is not straightforward, with an aging population, dwindling healthcare workforce and growing body of online health disinformation all conspiring against him.
As the proportion of Australians aged over 60 grows, conditions like dementia, heart disease and cancer — the latter of which affects nearly half of people by their 85th year — are expected to become more common. Along with them, the heat-induced and vector-borne illnesses that result from global warming.
And with vaccine hesitancy being fuelled online, there are fears conditions like measles could soon become widespread and see younger generations adding to the disease burden.
But, while Kidd acknowledges the challenges in front of him, he remains optimistic.
As the first GP to be appointed national CMO, Kidd — a former RACGP president — is wellplaced to support primary care, and is already involved in a range of reforms to this end.
Supporting the primary care workforce
“We are supporting primary healthcare professionals, through a range of incentives,” he said.
“Significant new investments from government to expand bulk billing are in place and will expand from 1 November under the new bulk billing practice incentive program.
“We expect that with additional and continued incentives it will become easier for all people to visit their GP.”
Junior doctors are also being incentivised to enter general practice, with more Commonwealth-supported university medical places, GP training opportunities, and pay and leave incentives.
There will be scholarships to support nurses and midwives training in primary care, and continued incentives for practitioners to work in underserved areas.
For those already in primary care, flexible working arrangements and opportunities
to support workers to fulfil their scope of practice will help improve quality of life.
“This will partly be achieved through our focus on multidisciplinary team models of care, which we know are effective in managing chronic conditions,” Kidd said.
“Through continued investment in the technologies that support integrated health care, it will become easier for GPs to coordinate with allied health, for example, and help individuals with complex comorbidities.”
However, it is not just disease management that will take up space in Kidd’s portfolio.
As the Department of Health, Disability and Ageing expands its remit to include disability, Kidd says there will be an increased emphasis on wellness and prevention, and better integration across the care sectors.
“Take aging. For me, this isn’t just about home-based or residential aged care programs. It’s an opportunity to focus on
healthy aging to support people to be as well as possible, for as long as possible,” he said.
Equity will feature in this prevention work, too, with Kidd focused on ensuring health research encompasses the needs of diverse population groups.
“We need to make sure that we are investing in research areas which reflect everyone in the population, so that we’re not leaving anyone behind.
“This builds on a strong push over recent years to invest in supporting improvements in the health of Aboriginal and Torres Strait Islander people; and particularly work with affected communities to make sure that research agendas are meeting the needs of communities and populations.”
Women’s health will also be prioritised, with female-specific and female-dominated health issues given further research investment.
“We will see continued investment in previously under-explored research areas and addressing gender bias in diagnostics and intervention,” Kidd said.
“That includes conditions that are more common in women, as well as conditions like endometriosis.”
While the Department’s goals may seem lofty, Kidd believes innovation could help drive exponential progress.
He is particularly excited about advances in genomics and their role in predicting health issues.
“We have been sitting on the cusp of a genomics revolution in clinical medicine for the last two decades — ever since the human genome project came to a conclusion,” he said.
“But what we haven’t seen is that translate into clinical practice. And I suspect over the coming decade or so we’re going to see that start to occur.”
At present, much of the work on genetics in clinical medicine is around single genes and their related conditions.
Soon, researchers will be able to examine a person’s entire genome and make more complex predictions, Kidd said.
“We are nearing the point where a person’s genome could be sequenced and become part of their health record, with that data then being utilised to help make decisions around health care, which is more personalised, precise and predictive,” he said.
While the challenges facing Australia’s health system may be formidable, Kidd’s forwardlooking response puts the Department in good stead to tackle them.
By embracing prevention, innovation and equity, Australia’s health system is set to uphold its reputation as one of the strongest, globally.
*Amy Sarcevic is a freelance science and technical writer who regularly writes for Hospital + Healthcare. She has an academic background in psychology.

MATHEW CHERIAN*
Australian-developed, cloud-based solutions have the potential to make digital health more accessible. A software-for-healthcare provider sets out some benefits.
Australian healthcare providers are under growing pressure to deliver high-quality, safe and efficient care amid rising patient demand, driven by an aging population and increasing rates of complex conditions. While digital health is often seen as the solution, implementation remains uneven — metropolitan public hospitals investing in large-scale system upgrades while regional areas may wait years for similar benefits.
Although digital health supporting clinicians is not a hugely new concept, the technology is still not being taken advantage of by the industry. From a lack of confidence to an outdated regulatory environment to experiencing ineffective and cookie-cutter solutions, there’s plenty holding decision-makers back.
Away from public institutions, private health care is also facing financial and competitive
pressures, subsequently limiting their capacity to adopt costly, monolithic technologies. There are Australian-built digital solutions available that offer a practical path forward that can ultimately massively boost both care quality and organisational performance; opportunities are plentiful, but a number of things need adjusting to enable our healthcare industry to push on and keep pace with other leading nations.
The problems
‘Greater expectations with fewer resources’: the healthcare industry is not the first to be a victim of this state of affairs. Digital health is often promoted as the solution to these challenges, but in reality, many organisations are struggling to implement systems that deliver real impact. There are a number of reasons as to why this is the case, but of key importance is that healthcare institutions’ key decision-makers lead the charge for digital
progress, or at the very least, are open to change; mindset and funding are often cited as the biggest barriers, but others also exist.
Unfortunately, there are some institutions that have been stung with ineffective and ill-fitting digital solutions, which has led to a reluctance to engage in alternative options. Whether these are global solutions that aren’t tailored to our nuanced healthcare system, one-size-fits-all solutions or simply poorly designed applications, these negative experiences can naturally impact future plans. In addition, the technology being developed is outpacing the regulatory environment we are currently operating in, which can present barriers to organisations looking to implement digital solutions.
The aim is to improve safety, efficiency and patient outcomes through the implementation

modernise services, stay competitive and respond more quickly to emerging clinical demands.
Currently, clinicians spend significant time on clerical tasks — searching for information, writing and rewriting notes — and are burdened by these. The consequence of this is that these clinicians are unable to dedicate as much time and energy as they’d like towards complex patient care, further straining already stretched resources and having a negative impact on job satisfaction and their own mental health. Smart digital systems being implemented can automate a lot of these routine tasks and free up clinicians’ time, helping to improve patient care.
Some SaaS (software-as-a-service) solutions are built to work with national healthcare frameworks such as My Health Record, while adhering to the Privacy Act 1988 and other Australian data protection laws. Some of these solutions also offer compliance tracking options, which can provide real-time visibility into compliance status across various regulations, affording users peace of mind and a level of automation for what can be a manual-heavy operation.
The national digital health policy must keep pace with technology to remove additional adoption barriers and should support incremental, scalable transformation rather than enforcing rigid, all-or-nothing system upgrades. There also needs to be a focus on encouraging and rewarding the use of Australian-built solutions as this will strengthen system alignment and compliance with local healthcare needs.
of digital solutions; however, there is still a divide between metro and rural institutions and the levels of service they are providing. Technology has the power to bridge this, but it requires a desire for change across the board. Metropolitan health services are replacing legacy systems with new digital platforms, offering a once-in-a-generation opportunity to redesign data collection and clinical workflows — while rural areas risk being left behind, with some regions facing severe wait times for equivalent upgrades.
Private providers must compete for patients while being constrained by insurer contracts and rising costs; they need to regularly update infrastructure and services but have limited appetite for costly, monolithic tech investments. Cloud-based, modular platforms offer a way forward, allowing private providers to buy only what they need and scale at their own pace. With the right technology, the private sector can
Cloud-based platforms reduce energy and resource demands as they don’t require maintenance, unlike on-premise infrastructure, while also allowing for costeffective, long-term scalability without repeated investments and upgrades to this infrastructure. Another aspect of the digital option is that it minimises paperbased workflows, which again lowers environmental impact and streamlines data handling.
Leading from the top
If digital tools are integrated properly into effective workflows, they can enable leadership teams to make informed decisions. This drives efficiency, removes manual processes, and improves both clinical outcomes and financial performance. With this, it’s crucial that these digital tools and the approach towards them in any organisation are led from the top — ensuring that sufficient training is provided and full employee buyin from the outset.
Key benefits of a cloudbased management system
• Disaster recovery and uptime guarantees. Unlike on-premise systems that can suffer unexpected failures or physical damage, SaaS platforms provide automated backups and disaster recovery plans. With climate change deemed a major risk to critical infrastructure in Australia, cloud-based solutions are less vulnerable to threats like flooding and bushfires. Many also have high uptime guarantees, exceeding 99.9% in some cases, ensuring continuous access to critical applications.
• Advanced cybersecurity protections. Cloud providers invest heavily in security, including multi-factor authentication, encryption and advanced threat detection, helping ensure data remains secure against breaches. So instead of security being all on the healthcare provider — necessitating help from an internal or external expert — moving to an SaaS platform can help achieve better data security and regulatory compliance without the need for constant in-house oversight.
• Reduced IT maintenance costs. With cloud-based systems, hospitals no longer need to maintain physical servers or continuously update outdated software. This reduction in maintenance allows IT teams to focus on more strategic projects — such as patient care initiatives, data analytics and strategic improvements. In other words, moving to an SaaS model allows hospitals to optimise IT resources while maintaining financial flexibility.
• Seamless interoperability. Modern SaaS solutions integrate effortlessly with existing hospital systems, third-party applications and national healthcare databases, improving efficiency and coordination.
• Real-time data sharing. Departments and external providers can access up-to-date patient records, enhancing communication and reducing redundancy in care.
• Automatic updates and futureproofing. SaaS providers continuously update and improve their platforms, so hospitals benefit from the latest innovations without